Stimulates The Interstitial Cells Of The Testes To Secrete
Juapaving
Mar 30, 2025 · 5 min read
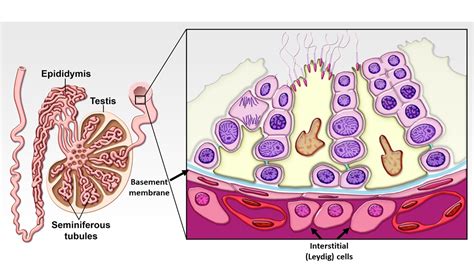
Table of Contents
Stimulates the Interstitial Cells of the Testes to Secrete: A Deep Dive into Testosterone Production and Regulation
The intricate process of testosterone production involves a complex interplay of hormones and cellular mechanisms within the testes. Understanding how the interstitial cells of Leydig (ICL), also known as Leydig cells, are stimulated to secrete testosterone is crucial for comprehending male reproductive health, sexual development, and overall well-being. This comprehensive article delves into the mechanisms that govern this vital process, exploring the key players, regulatory pathways, and the implications of dysregulation.
The Role of the Interstitial Cells of Leydig (ICL)
The ICL are specialized endocrine cells located within the interstitial spaces of the testes, nestled between the seminiferous tubules where sperm production occurs. Their primary function is the synthesis and secretion of testosterone, the principal male sex hormone. Testosterone plays a multifaceted role, influencing:
-
Sexual Development: From fetal development to puberty, testosterone orchestrates the differentiation of male reproductive organs and the development of secondary sexual characteristics such as increased muscle mass, bone density, and the growth of facial and body hair.
-
Spermatogenesis: While not directly involved in sperm production, testosterone supports spermatogenesis by creating the hormonal environment necessary for the process to occur effectively within the seminiferous tubules.
-
Sexual Function: Testosterone is essential for maintaining libido, erectile function, and overall sexual health.
-
Metabolic Processes: Testosterone influences metabolic rate, body composition, and bone health.
The Master Regulator: Luteinizing Hormone (LH)
The primary stimulus for testosterone secretion from the ICL is luteinizing hormone (LH), a gonadotropin hormone produced by the anterior pituitary gland in the brain. The hypothalamus, the control center of the endocrine system, releases gonadotropin-releasing hormone (GnRH), which triggers the pituitary gland to release LH. This process is tightly regulated through a feedback loop involving testosterone levels.
The LH Receptor and the cAMP Pathway
LH exerts its effect by binding to specific LH receptors located on the surface of the ICL. This binding initiates a cascade of intracellular events, primarily involving the cyclic adenosine monophosphate (cAMP) signaling pathway.
-
LH Binding: LH binds to its receptor, causing a conformational change.
-
G-protein Activation: This change activates a G-protein coupled receptor, initiating a series of downstream events.
-
Adenylate Cyclase Activation: The activated G-protein stimulates adenylate cyclase, an enzyme that converts ATP to cAMP.
-
cAMP-dependent Protein Kinase A (PKA) Activation: The increased cAMP levels activate protein kinase A (PKA), a crucial enzyme that phosphorylates various proteins.
-
Steroidogenic Acute Regulatory Protein (StAR) Induction: One of the key proteins phosphorylated by PKA is the StAR protein. StAR is crucial for the transport of cholesterol into the mitochondria, the powerhouse of the cell. Cholesterol is the precursor for testosterone synthesis.
-
Testosterone Synthesis: Within the mitochondria, a series of enzymatic reactions, collectively known as steroidogenesis, convert cholesterol into testosterone. These enzymes include cytochrome P450 side-chain cleavage enzyme (CYP11A1), 17α-hydroxylase/17,20-lyase (CYP17A1), and 17β-hydroxysteroid dehydrogenase (17β-HSD).
Other Factors Influencing Testosterone Secretion
While LH is the primary regulator, other factors can modulate testosterone production:
-
Follicle-stimulating Hormone (FSH): Although primarily known for its role in spermatogenesis, FSH can indirectly influence testosterone production by supporting Sertoli cell function, which in turn influences the production of factors that can impact ICL function.
-
Growth Factors: Various growth factors, such as insulin-like growth factor 1 (IGF-1) and fibroblast growth factor (FGF), have been shown to modulate ICL function and testosterone production. These factors often act synergistically with LH.
-
Cytokines: Inflammatory cytokines, such as tumor necrosis factor-alpha (TNF-α) and interleukin-1 (IL-1), can negatively impact ICL function and reduce testosterone production. Chronic inflammation can thus contribute to lower testosterone levels.
-
Age: Testosterone production naturally declines with age, a phenomenon known as andropause or late-onset hypogonadism. This age-related decline is attributed to a decrease in LH secretion and a reduced responsiveness of ICL to LH stimulation.
-
Nutritional Status: Adequate nutrition, particularly sufficient intake of protein, zinc, and vitamin D, is essential for maintaining optimal testosterone production. Deficiencies in these nutrients can impair ICL function.
-
Lifestyle Factors: Lifestyle choices like smoking, excessive alcohol consumption, and lack of physical activity can negatively affect testosterone levels. Obesity is strongly associated with reduced testosterone production due to increased aromatization of testosterone to estrogen.
Regulation Through Negative Feedback
The hypothalamic-pituitary-testicular axis operates under a delicate negative feedback system. Elevated testosterone levels inhibit the release of GnRH from the hypothalamus and LH from the pituitary gland, thereby reducing further testosterone production. Conversely, low testosterone levels stimulate the release of GnRH and LH, increasing testosterone synthesis. This feedback loop helps maintain testosterone levels within a physiological range.
Clinical Implications of ICL Dysfunction
Dysfunction of the ICL can lead to various clinical conditions, including:
-
Hypogonadism: This condition is characterized by abnormally low levels of testosterone, leading to a range of symptoms including decreased libido, erectile dysfunction, fatigue, reduced muscle mass, and osteoporosis.
-
Infertility: Impaired testosterone production can negatively impact spermatogenesis, contributing to infertility.
-
Delayed Puberty: Insufficient testosterone production during puberty can result in delayed or incomplete development of secondary sexual characteristics.
-
Certain Cancers: Some types of testicular cancer may be associated with altered ICL function.
Conclusion: A Symphony of Hormonal Regulation
The stimulation of interstitial cells of the testes to secrete testosterone is a finely tuned process, regulated by a complex interplay of hormonal and cellular mechanisms. LH serves as the primary driver, initiating a cascade of events that culminates in testosterone synthesis. However, other factors, including FSH, growth factors, cytokines, age, nutrition, and lifestyle, significantly modulate this process. Understanding this intricate regulation is crucial for developing effective diagnostic and therapeutic strategies for conditions associated with ICL dysfunction. Further research continues to illuminate the complexities of testosterone production, paving the way for improved management of related health concerns. Maintaining a healthy lifestyle, including regular exercise, a balanced diet, and stress management, is crucial for supporting optimal testosterone levels and overall well-being. In cases of suspected ICL dysfunction, seeking professional medical evaluation is essential for appropriate diagnosis and treatment.
Latest Posts
Latest Posts
-
Finding Area Under A Curve Calculator
Apr 01, 2025
-
Are Polar Bonds Stronger Than Nonpolar
Apr 01, 2025
-
Lowest Common Multiple Of 15 And 25
Apr 01, 2025
-
Blood Is A Compound Or Mixture
Apr 01, 2025
-
Compare And Contrast Hinduism And Buddhism
Apr 01, 2025
Related Post
Thank you for visiting our website which covers about Stimulates The Interstitial Cells Of The Testes To Secrete . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
