Label The Diagram Of The Male Reproductive System
Juapaving
Mar 29, 2025 · 7 min read
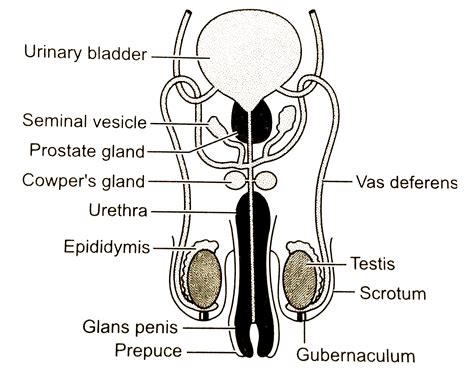
Table of Contents
Label the Diagram of the Male Reproductive System: A Comprehensive Guide
Understanding the male reproductive system is crucial for overall health and well-being. This detailed guide will walk you through the anatomy of the male reproductive system, providing a comprehensive explanation of each part and its function. We'll also provide a clear, labeled diagram to help you visualize and understand the complex interplay of these organs.
The Major Components of the Male Reproductive System
The male reproductive system is responsible for producing, storing, and transporting sperm, the male gametes, and delivering them to the female reproductive tract for fertilization. This system consists of several key organs working in concert:
1. Testes (Testicles): The Sperm Factories
Function: The testes are the primary male reproductive organs. Their primary function is spermatogenesis, the process of producing sperm. They are also responsible for the production of testosterone, the primary male sex hormone, crucial for sexual development and secondary sexual characteristics.
Structure: Each testis is an oval-shaped organ housed within the scrotum. Inside the testes are tightly coiled seminiferous tubules where sperm production takes place. Interstitial cells (Leydig cells) located between the tubules produce testosterone.
Importance: Healthy testes are essential for fertility. Any impairment in their function can lead to infertility or hormonal imbalances.
2. Scrotum: Protecting the Testicles
Function: The scrotum is a sac-like structure that holds the testes externally. Its primary function is temperature regulation. Sperm production requires a temperature slightly lower than the core body temperature. The scrotum's muscles contract and relax to adjust the distance of the testes from the body, maintaining the optimal temperature for spermatogenesis.
Structure: The scrotum is composed of skin and muscle tissue. The dartos muscle within the scrotum is responsible for wrinkling the scrotal skin, which helps regulate temperature. The cremaster muscle raises and lowers the testes to maintain optimal temperature.
Importance: Maintaining the correct scrotal temperature is crucial for sperm viability and fertility. Conditions that interfere with scrotal temperature regulation can negatively impact sperm production.
3. Epididymis: Maturation and Storage
Function: The epididymis is a long, coiled tube located on the posterior surface of each testis. Its primary function is the maturation and storage of sperm. Sperm produced in the testes are immature and non-motile. They spend several days in the epididymis where they mature and gain the ability to swim. The epididymis also reabsorbs excess fluid, concentrating the sperm.
Structure: The epididymis consists of a head, body, and tail. The head receives sperm from the efferent ductules of the testes, the body is where maturation occurs, and the tail stores mature sperm.
Importance: The epididymis is vital for sperm maturation and fertility. Problems with epididymal function can lead to reduced sperm motility and infertility.
4. Vas Deferens (Ductus Deferens): Transporting Sperm
Function: The vas deferens is a muscular tube that transports mature sperm from the epididymis to the ejaculatory duct. Peristaltic contractions of the vas deferens propel the sperm during ejaculation.
Structure: The vas deferens is a thick-walled tube extending from the epididymis, passing through the inguinal canal, and up into the pelvic cavity. It joins with the seminal vesicle to form the ejaculatory duct.
Importance: The vas deferens is essential for sperm delivery to the urethra. A vasectomy, a procedure that cuts and ties the vas deferens, is a common form of male sterilization.
5. Seminal Vesicles: Providing Nutrients
Function: The seminal vesicles are two sac-like glands located behind the bladder. They produce a viscous, alkaline fluid that makes up about 60% of the semen volume. This fluid contains fructose, which provides energy for sperm, and prostaglandins, which may aid in sperm motility and fertilization.
Structure: The seminal vesicles are highly vascularized glands with a complex network of tubules.
Importance: The seminal vesicle fluid is essential for sperm survival and motility.
6. Prostate Gland: Adding Volume and Nutrients
Function: The prostate gland is a walnut-sized gland located below the bladder that surrounds the urethra. It produces a milky, slightly alkaline fluid that makes up about 25-30% of semen volume. This fluid contains enzymes that enhance sperm motility and neutralize the acidity of the vagina.
Structure: The prostate gland is made up of smooth muscle and glandular tissue.
Importance: The prostate gland's secretions are crucial for sperm survival and successful fertilization. Enlarged prostate glands (benign prostatic hyperplasia) are common in older men and can cause urinary problems.
7. Bulbourethral Glands (Cowper's Glands): Pre-Ejaculate
Function: The bulbourethral glands are two small pea-sized glands located below the prostate gland. They secrete a clear, viscous fluid that lubricates the urethra and neutralizes any residual acidity before ejaculation. This pre-ejaculate may contain a small number of sperm.
Structure: The bulbourethral glands are composed of mucous-secreting cells.
Importance: Bulbourethral gland secretions prepare the urethra for the passage of semen, and the pre-ejaculate helps to neutralize the acidity of the urethra.
8. Urethra: The Passageway
Function: The urethra is the tube that carries urine from the bladder and semen from the reproductive system out of the body through the penis.
Structure: The urethra passes through the prostate gland and penis.
Importance: The urethra serves as a shared passageway for both the urinary and reproductive systems.
9. Penis: Delivery Mechanism
Function: The penis is the male organ of copulation. It delivers sperm to the female reproductive tract during sexual intercourse. It also serves as the outlet for urine.
Structure: The penis consists of three cylindrical masses of erectile tissue (two corpora cavernosa and one corpus spongiosum) surrounded by a sheath of fibrous tissue and skin. During sexual arousal, these tissues become engorged with blood, causing an erection.
Importance: The penis is essential for sexual intercourse and the delivery of sperm for fertilization.
Diagram of the Male Reproductive System (with labels)
(Insert a high-quality, clearly labeled diagram here. The diagram should show all the organs listed above with clear labels for each. This is crucial for visual understanding and is a key SEO element. Consider using a vector-based image format for high resolution.)
Common Conditions Affecting the Male Reproductive System
Several conditions can affect the male reproductive system, impacting fertility and overall health. Some common examples include:
- Testicular Cancer: A cancerous tumor arising from the cells within the testes.
- Prostatitis: Inflammation of the prostate gland, which can cause pain, urinary problems, and sexual dysfunction.
- Prostate Cancer: A cancer of the prostate gland, one of the most common cancers in men.
- Erectile Dysfunction: The inability to achieve or maintain an erection sufficient for satisfactory sexual intercourse.
- Infertility: The inability to conceive a child. This can be due to various factors affecting the production, transport, or function of sperm.
- Varicocele: An enlargement of the veins within the scrotum. This can impair testicular temperature regulation and affect sperm production.
- Hydrocele: A fluid-filled sac surrounding the testicle.
- Inguinal Hernia: A protrusion of abdominal contents through a weakness in the abdominal wall, often near the inguinal canal.
Maintaining Reproductive Health
Maintaining good reproductive health is essential for men of all ages. Key steps include:
- Regular self-exams: Regular self-examination of the testes can help detect lumps or abnormalities early.
- Healthy lifestyle: Maintaining a healthy weight, eating a balanced diet, and regular exercise contribute to overall health, including reproductive health.
- Avoiding smoking and excessive alcohol consumption: These habits negatively impact reproductive health.
- Seeking medical attention: If you experience any symptoms such as pain, swelling, or changes in urination or sexual function, consult a doctor promptly.
Conclusion: A Deeper Understanding
This comprehensive guide provides a detailed overview of the male reproductive system, highlighting the structure and function of each component. Understanding this system is crucial for maintaining good health and addressing potential issues promptly. Remember that regular self-checks, a healthy lifestyle, and timely medical attention are key to maintaining optimal reproductive health. The inclusion of a high-quality, labeled diagram serves as a powerful visual aid, enhancing understanding and making this a valuable resource for students, healthcare professionals, and anyone interested in learning more about male reproductive anatomy. By incorporating comprehensive information, clear visuals, and addressing common concerns, this article aims to be a highly informative and valuable resource for a broad audience. This detailed approach optimizes the article for SEO purposes, targeting relevant keywords and phrases to increase visibility and accessibility.
Latest Posts
Latest Posts
-
How Many Valence Electrons Are In H2o
Mar 31, 2025
-
51 Cm Is How Many Inches
Mar 31, 2025
-
A Rectangle Is Sometimes A Square
Mar 31, 2025
-
The Two Purines In Dna Are
Mar 31, 2025
-
A To Z In Cursive Writing
Mar 31, 2025
Related Post
Thank you for visiting our website which covers about Label The Diagram Of The Male Reproductive System . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
