What Is The Principal Cation Of The Ecf
Juapaving
Mar 22, 2025 · 5 min read
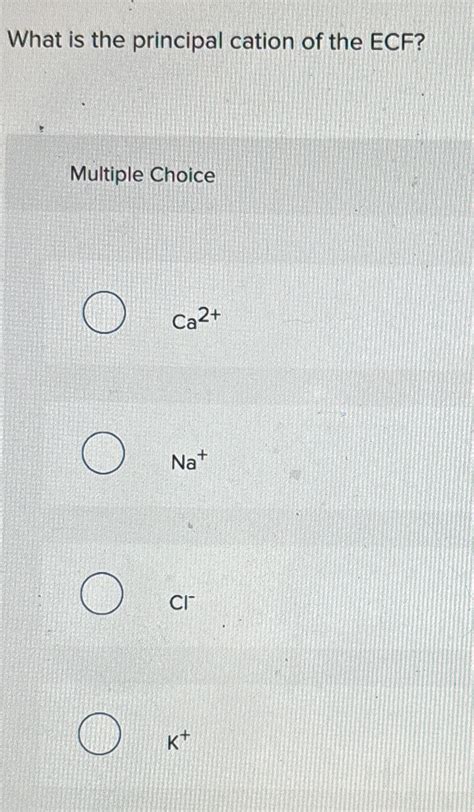
Table of Contents
What is the Principal Cation of the ECF? Understanding Sodium's Crucial Role
The extracellular fluid (ECF) is the body's vital transport system, carrying nutrients, hormones, and waste products. Maintaining its precise composition is crucial for life. A key component of this composition is the balance of electrolytes, charged particles that play critical roles in numerous bodily functions. While many ions contribute, the principal cation of the ECF is undoubtedly sodium (Na+). This article will delve into the significance of sodium in the ECF, exploring its functions, regulation, and the consequences of imbalance.
Sodium's Dominance in the Extracellular Fluid
Sodium ions represent the most abundant cation in the ECF, significantly outnumbering other positive ions like potassium, calcium, and magnesium. This dominance is not accidental; it's essential for a multitude of physiological processes. The concentration of sodium in the ECF is tightly regulated, typically around 135-145 mEq/L. This narrow range is crucial because even slight deviations can have profound effects on various bodily systems.
Why is Sodium the Principal Cation?
Sodium's role as the principal ECF cation stems from several factors:
-
Water Balance: Sodium plays a pivotal role in regulating the body's water balance. Through osmosis, water moves across cell membranes to equalize the concentration of solutes. Because sodium is the most abundant solute in the ECF, it exerts a significant osmotic pressure, drawing water into the extracellular compartment. This relationship is crucial for maintaining blood volume and blood pressure.
-
Electrochemical Gradients: The difference in sodium concentration between the ECF and intracellular fluid (ICF) contributes to the electrochemical gradients across cell membranes. These gradients are essential for various cellular processes, including nerve impulse transmission, muscle contraction, and nutrient transport. The sodium-potassium pump, a critical membrane protein, actively transports sodium out of cells and potassium into cells, maintaining these crucial gradients.
-
Acid-Base Balance: Sodium participates in acid-base regulation, influencing the body's pH. Sodium bicarbonate (NaHCO3), a major buffer in the ECF, helps to neutralize excess acids, preventing significant changes in blood pH.
-
Nutrient Absorption: Sodium plays a key role in the absorption of glucose and amino acids from the digestive tract. Sodium co-transporters in the intestinal lining facilitate the movement of these nutrients into the bloodstream.
Sodium Regulation: A Delicate Balance
The body employs several sophisticated mechanisms to maintain sodium homeostasis, ensuring that its concentration in the ECF remains within the narrow physiological range. These mechanisms involve:
1. Renal Regulation: The Kidneys' Crucial Role
The kidneys are the primary regulators of sodium balance. They control sodium excretion through several processes:
-
Glomerular Filtration: Sodium is freely filtered at the glomerulus, the initial filtering unit of the nephron.
-
Tubular Reabsorption: The majority of filtered sodium is reabsorbed in the proximal tubule, primarily through active transport mechanisms driven by the sodium-potassium pump. This reabsorption is highly regulated, influenced by hormones like aldosterone.
-
Tubular Secretion: A small amount of sodium can be secreted into the nephron tubules, but this is typically a minor contributor to overall sodium excretion.
-
Hormonal Influence: Several hormones influence renal sodium handling:
-
Aldosterone: This hormone, secreted by the adrenal glands, stimulates sodium reabsorption in the distal tubule and collecting duct, increasing sodium retention and blood volume. It's particularly important in situations of low blood volume or low sodium levels.
-
Antidiuretic Hormone (ADH): While primarily involved in water balance, ADH indirectly affects sodium concentration by influencing water reabsorption. Increased ADH leads to increased water reabsorption, potentially diluting the sodium concentration.
-
Atrial Natriuretic Peptide (ANP): This hormone, secreted by the heart in response to increased blood volume, promotes sodium excretion by inhibiting sodium reabsorption in the kidney.
-
2. Other Regulatory Mechanisms
Besides renal regulation, other mechanisms contribute to sodium homeostasis:
-
Thirst Mechanism: When sodium levels are high, the body experiences thirst, prompting fluid intake to dilute the ECF.
-
Gastrointestinal Tract: The gastrointestinal tract plays a minor role in sodium absorption and excretion.
Consequences of Sodium Imbalance
Maintaining sodium balance is paramount for health. Both hyponatremia (low sodium) and hypernatremia (high sodium) can lead to serious health consequences.
Hyponatremia: The Dangers of Low Sodium
Hyponatremia, characterized by a serum sodium concentration below 135 mEq/L, can result from several factors:
-
Excessive Water Intake: Drinking excessive amounts of water can dilute the sodium concentration in the ECF.
-
Diuretic Use: Certain diuretics increase sodium excretion, potentially leading to hyponatremia.
-
Kidney Failure: Impaired kidney function can hinder sodium reabsorption.
-
Hormonal Imbalances: Conditions like syndrome of inappropriate antidiuretic hormone secretion (SIADH) can cause excessive water retention, resulting in hyponatremia.
Symptoms of hyponatremia can range from mild (headache, nausea) to severe (seizures, coma). Treatment focuses on correcting the underlying cause and restoring fluid balance.
Hypernatremia: The Effects of High Sodium
Hypernatremia, defined as a serum sodium concentration above 145 mEq/L, typically reflects water loss or excessive sodium intake. Causes include:
-
Dehydration: Severe dehydration, due to inadequate fluid intake or excessive fluid loss (e.g., diarrhea, vomiting), can lead to a relative increase in sodium concentration.
-
Excessive Sodium Intake: Consuming excessive amounts of sodium, particularly through a high-salt diet, can contribute to hypernatremia.
-
Diabetes Insipidus: This condition, characterized by a deficiency in ADH, leads to excessive water excretion, resulting in hypernatremia.
Symptoms of hypernatremia often involve neurological manifestations, including confusion, seizures, and coma. Treatment aims to restore fluid balance through careful fluid administration.
Clinical Significance and Monitoring
Precise monitoring of serum sodium levels is essential in clinical settings. Regular electrolyte panels are crucial for patients with various medical conditions, including kidney disease, heart failure, and endocrine disorders. Careful attention to sodium intake and fluid balance is vital in preventing and managing sodium imbalances.
Conclusion: Sodium's Indispensable Role
Sodium, the principal cation of the ECF, plays a crucial role in maintaining fluid balance, electrochemical gradients, acid-base balance, and nutrient absorption. The body employs sophisticated regulatory mechanisms to maintain sodium homeostasis within a narrow physiological range. Disruptions in this balance, leading to hyponatremia or hypernatremia, can have serious health consequences, highlighting the critical importance of sodium in overall health and well-being. Understanding sodium's multifaceted functions and the mechanisms that regulate its levels is fundamental to comprehending human physiology and clinical medicine. Furthermore, ongoing research continues to unravel the complexities of sodium homeostasis, paving the way for improved diagnostic and therapeutic approaches to sodium-related disorders. The significance of sodium's role as the principal cation of the ECF cannot be overstated; it's an ion that truly underpins life itself.
Latest Posts
Latest Posts
-
Whats The Prime Factorization Of 64
Mar 22, 2025
-
Compound Simple And Complex Sentences Worksheet
Mar 22, 2025
-
The Hydrolysis Of Atp Yields Adp Phosphate Ion And
Mar 22, 2025
-
Is Sodium Carbonate The Same As Baking Soda
Mar 22, 2025
-
How To Convert Pka To Ph
Mar 22, 2025
Related Post
Thank you for visiting our website which covers about What Is The Principal Cation Of The Ecf . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
