The Only Movable Joint In The Skull Is Between The
Juapaving
Mar 27, 2025 · 7 min read
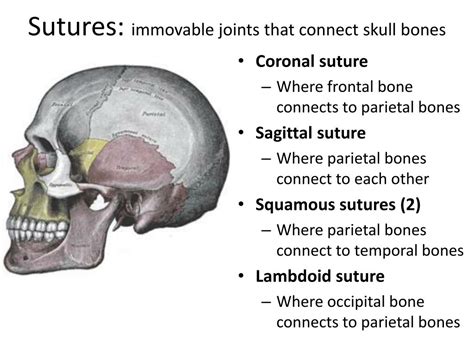
Table of Contents
The Only Movable Joint in the Skull: The Temporomandibular Joint (TMJ)
The human skull, a complex and fascinating structure, is largely composed of immovable joints, also known as sutures. These fibrous joints fuse the various cranial bones together, providing robust protection for the brain. However, one crucial exception exists: the temporomandibular joint (TMJ). This unique joint, located on each side of the head, is the only movable joint in the skull, enabling the essential functions of speaking, chewing, and yawning. Understanding the TMJ's anatomy, function, and potential disorders is crucial for appreciating the intricate mechanics of the human head and neck.
Anatomy of the Temporomandibular Joint (TMJ)
The TMJ is a complex synovial joint, classified as a ginglymoarthrodial joint, meaning it possesses characteristics of both a hinge joint (ginglymus) and a gliding joint (arthrodial). This dual functionality allows for a wide range of movements, including hinge-like opening and closing of the mouth, and gliding movements involved in protrusion, retraction, and lateral movement (side-to-side chewing).
Several key anatomical structures contribute to the TMJ's function:
1. Mandibular Condyle:
The mandibular condyle, a rounded projection at the end of the mandible (lower jawbone), articulates with the temporal bone of the skull. Its shape and smooth articular surface are crucial for efficient joint movement.
2. Mandibular Fossa and Articular Eminence:
The temporal bone provides the receiving socket for the mandibular condyle. The mandibular fossa is a concave depression, and the articular eminence is an anterior bony ridge that guides the condylar movement during jaw opening and closing.
3. Articular Disc (Meniscus):
A crucial component of the TMJ is the articular disc, a biconcave fibrocartilaginous structure that sits between the mandibular condyle and the temporal bone. This disc acts as a shock absorber, distributing forces evenly across the joint, and also facilitates smooth movement by dividing the joint into two separate compartments:
- Superior joint cavity: Lies between the disc and the temporal bone. Primarily involved in gliding movements.
- Inferior joint cavity: Situated between the disc and the condyle. Primarily involved in hinge movements.
4. Joint Capsule:
The entire TMJ is enclosed by a fibrous joint capsule, which provides stability and support. This capsule is lined with a synovial membrane, which secretes synovial fluid. This fluid lubricates the joint surfaces, reducing friction and ensuring smooth movement.
5. Ligaments:
Several ligaments reinforce the TMJ, providing stability and restricting excessive movement. Key ligaments include:
- Temporomandibular ligament: The main supporting ligament, preventing excessive opening and posterior displacement of the condyle.
- Stylomandibular ligament: A collateral ligament that provides support but is not directly involved in primary TMJ function.
- Sphenomandibular ligament: A vestigial ligament with minimal functional importance in the TMJ.
Function of the Temporomandibular Joint (TMJ)
The TMJ's primary function is to enable the intricate movements of the mandible, facilitating essential tasks such as:
-
Mastication (chewing): The TMJ allows for the precise movements required to grind and crush food. This involves both hinge and gliding actions, enabling the mandible to move up and down, side-to-side, and forward and backward.
-
Speech: Clear and articulate speech depends on the precise and coordinated movements of the mandible, controlled by the TMJ. Sounds requiring jaw movement, such as consonants like "b," "p," and "m," rely heavily on TMJ function.
-
Yawning: The wide opening of the mouth during yawning also necessitates the full range of TMJ motion.
Disorders Affecting the Temporomandibular Joint (TMJ)
Despite its robust structure, the TMJ is susceptible to various disorders, collectively known as temporomandibular joint disorders (TMD). These disorders can cause significant pain and dysfunction, affecting daily activities. Common TMDs include:
1. Temporomandibular Joint Pain:
This manifests as pain in the TMJ region, often accompanied by tenderness to the touch. The pain can radiate to other areas, such as the ear, temple, or jaw.
2. TMJ Clicks and Pops:
These audible sounds often accompany jaw movement and can indicate joint dysfunction, such as disc displacement or degenerative changes.
3. Limited Jaw Opening:
Difficulty opening the mouth widely can be a significant symptom of TMD. This limitation is often accompanied by pain and discomfort.
4. TMJ Locking:
In some cases, the jaw can become completely locked, unable to open or close. This necessitates immediate medical attention.
5. Myofascial Pain:
Pain originating from the muscles of mastication (chewing muscles) is frequently associated with TMJ disorders. These muscles can become tense and painful due to overuse, stress, or poor posture.
Causes of Temporomandibular Joint Disorders (TMD)
The etiology of TMD is often multifactorial, meaning multiple factors contribute to its development. Some key contributing factors include:
-
Trauma: Direct injury to the jaw or TMJ can lead to joint damage and dysfunction.
-
Arthritis: Degenerative joint diseases, such as osteoarthritis or rheumatoid arthritis, can affect the TMJ, causing pain, inflammation, and stiffness.
-
Bruxism: The involuntary grinding or clenching of teeth, often occurring during sleep, puts excessive strain on the TMJ, leading to wear and tear and pain.
-
Stress: Psychological stress can contribute to TMD by increasing muscle tension and potentially exacerbating existing joint issues.
-
Poor Posture: Maintaining poor posture can strain the muscles supporting the TMJ, leading to discomfort and pain.
-
Genetics: A family history of TMD might increase one's susceptibility.
Diagnosis and Treatment of Temporomandibular Joint Disorders (TMD)
Diagnosing TMD involves a comprehensive clinical examination, including a thorough history, physical examination of the TMJ, and assessment of jaw movement. Imaging techniques, such as X-rays, MRI, or CT scans, may be used to visualize the joint structures and identify any abnormalities.
Treatment options for TMD vary depending on the severity and underlying cause. Conservative management strategies often include:
-
Pain Management: Over-the-counter pain relievers, such as ibuprofen or acetaminophen, can help alleviate pain and inflammation. In some cases, stronger prescription pain medications may be necessary.
-
Physical Therapy: Specialized exercises and therapies can strengthen the jaw muscles, improve joint mobility, and reduce pain.
-
Splints or Mouthguards: These devices can help alleviate pain by realigning the jaw, reducing muscle tension, and protecting the teeth from grinding.
-
Lifestyle Modifications: Reducing stress, improving posture, and adopting a healthy diet can contribute to improved TMJ health.
In cases where conservative treatment fails, surgical intervention may be considered. Surgical options range from minimally invasive arthroscopic procedures to more extensive reconstructive surgeries.
Prevention of Temporomandibular Joint Disorders (TMD)
While not all TMD cases are preventable, adopting proactive measures can significantly reduce the risk of developing these disorders. These preventative strategies include:
-
Stress Management: Practicing stress-reducing techniques, such as yoga, meditation, or deep breathing exercises, can help minimize muscle tension and reduce the risk of TMD.
-
Maintaining Good Posture: Consciously maintaining good posture while sitting, standing, and sleeping can lessen the strain on the jaw muscles and TMJ.
-
Treating Bruxism: If you grind or clench your teeth, a mouthguard worn at night can protect your teeth and alleviate stress on the TMJ.
-
Eating a Healthy Diet: Maintaining a well-balanced diet can improve overall health and potentially minimize factors contributing to TMJ problems.
-
Gentle Jaw Exercises: Performing gentle jaw exercises can help improve jaw mobility and reduce muscle tension. Consult with a physical therapist for appropriate exercises.
Conclusion: The Vital Role of the TMJ
The temporomandibular joint, the only movable joint in the skull, plays a vital role in everyday life, enabling essential functions such as eating, speaking, and yawning. Understanding the anatomy, function, and potential disorders of the TMJ is crucial for appreciating its significance and for effectively managing the often painful and debilitating conditions that can affect this unique joint. By adopting a proactive approach to maintaining TMJ health through lifestyle modifications, stress management, and prompt treatment of any developing issues, individuals can protect this vital joint and maintain its optimal functionality throughout their lives. Early intervention and a holistic approach, integrating various treatment modalities where necessary, are essential for ensuring a positive outcome in managing TMJ disorders and restoring quality of life.
Latest Posts
Latest Posts
-
Find The Area Under The Curve Calculator
Mar 30, 2025
-
Is Butter Melting A Physical Change
Mar 30, 2025
-
How Many Cm Are In 12 Inches
Mar 30, 2025
-
What Metals Are The Most Reactive
Mar 30, 2025
-
Common Denominator Of 8 And 3
Mar 30, 2025
Related Post
Thank you for visiting our website which covers about The Only Movable Joint In The Skull Is Between The . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
