Glomerular Hydrostatic Pressure Is The Pressure Of
Juapaving
Mar 21, 2025 · 6 min read
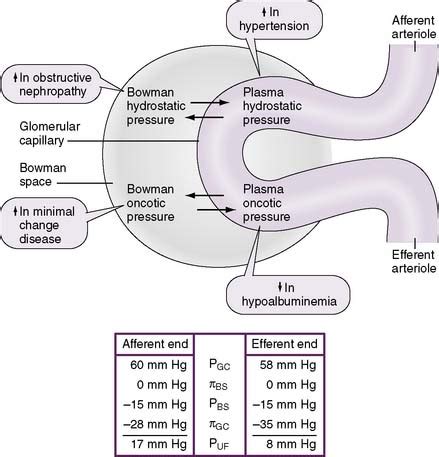
Table of Contents
Glomerular Hydrostatic Pressure: The Pressure Driving Filtration in the Kidneys
The kidneys are remarkable organs responsible for filtering waste products from the blood, maintaining electrolyte balance, and regulating blood pressure. Understanding the intricate mechanisms within the nephron, the functional unit of the kidney, is crucial to appreciating the overall function of the renal system. A key player in this process is glomerular hydrostatic pressure (GHP). This article delves deep into what GHP is, its role in glomerular filtration, the factors influencing it, and the consequences of its dysregulation.
What is Glomerular Hydrostatic Pressure (GHP)?
Glomerular hydrostatic pressure is the blood pressure within the glomerular capillaries of the nephron. It's the driving force behind glomerular filtration, the initial and critical step in urine formation. Think of it as the pressure pushing blood against the semi-permeable membrane of the glomerulus, forcing water and small dissolved solutes into Bowman's capsule, the initial collecting point of the filtrate. This pressure is significantly higher than capillary pressure in other parts of the body, reflecting the unique structure and function of the glomerulus. This higher pressure is essential for efficient filtration.
The Glomerulus: A Specialized Filtration Unit
The glomerulus is a network of specialized capillaries nestled within Bowman's capsule. Its unique structure is tailored for efficient filtration. The capillaries possess fenestrations, or pores, allowing the passage of water and small molecules while restricting the passage of larger proteins and blood cells. This selective permeability is crucial for maintaining the integrity of the blood while efficiently filtering waste products. The afferent arteriole, supplying blood to the glomerulus, is larger in diameter than the efferent arteriole, which carries blood away. This difference in diameter contributes significantly to the high GHP.
The Role of GHP in Glomerular Filtration
GHP plays a central role in the process of glomerular filtration. The filtration process is governed by Starling's forces, a balance of hydrostatic and osmotic pressures acting across the glomerular membrane. GHP is one of these crucial forces. In simple terms, the higher the GHP, the greater the volume of filtrate formed. This directly translates to the rate of filtration, a critical aspect of renal function. The equation governing filtration is expressed as:
Net Filtration Pressure (NFP) = GHP - (CHP + BCOP)
Where:
- GHP = Glomerular Hydrostatic Pressure
- CHP = Capsular Hydrostatic Pressure (pressure in Bowman's capsule)
- BCOP = Bowman's Capsule Osmotic Pressure (pressure due to proteins in Bowman's capsule)
Understanding the Components of Net Filtration Pressure
-
GHP: As discussed, this is the primary driving force pushing fluid out of the glomerular capillaries. Normally, GHP is approximately 55 mmHg.
-
CHP: This is the hydrostatic pressure exerted by the fluid already present in Bowman's capsule. It opposes filtration and is typically around 15 mmHg.
-
BCOP: This reflects the osmotic pressure exerted by proteins within Bowman's capsule. Since relatively few proteins are filtered, this pressure is normally low (around 0 mmHg, but can be slightly higher).
Consequently, the net filtration pressure (NFP) is usually around 40 mmHg, which effectively represents the driving force for filtration.
Factors Affecting Glomerular Hydrostatic Pressure
Several factors can influence GHP, ultimately affecting the glomerular filtration rate (GFR). Understanding these factors is crucial for diagnosing and managing renal dysfunction.
1. Systemic Blood Pressure
A crucial factor determining GHP is systemic blood pressure. An increase in systemic blood pressure directly translates to a higher GHP, leading to increased GFR. Conversely, a decrease in systemic blood pressure results in lower GHP and reduced GFR. This relationship highlights the interplay between cardiovascular and renal systems.
2. Afferent and Efferent Arteriole Diameter
The diameter of both the afferent and efferent arterioles significantly impacts GHP.
-
Afferent Arteriole Constriction: Decreases blood flow into the glomerulus, reducing GHP and GFR.
-
Afferent Arteriole Dilation: Increases blood flow into the glomerulus, increasing GHP and GFR.
-
Efferent Arteriole Constriction: Reduces blood outflow from the glomerulus, increasing GHP and GFR.
-
Efferent Arteriole Dilation: Increases blood outflow from the glomerulus, decreasing GHP and GFR. This intricate regulation allows for fine-tuning of GFR.
3. Renal Autoregulation
The kidneys possess an intrinsic ability to maintain a relatively constant GFR despite fluctuations in systemic blood pressure. This process, known as renal autoregulation, involves myogenic and tubuloglomerular feedback mechanisms. These mechanisms adjust afferent and efferent arteriolar diameters to counteract changes in systemic blood pressure, maintaining a stable GHP within a certain range.
4. Hormonal Influences
Several hormones play a role in regulating GHP and GFR.
-
Angiotensin II: A potent vasoconstrictor, predominantly constricting the efferent arteriole, increases GHP and GFR. However, at high levels, it can also constrict the afferent arteriole, decreasing GFR.
-
Atrial Natriuretic Peptide (ANP): Promotes vasodilation of both afferent and efferent arterioles, indirectly affecting GHP and GFR. The overall effect is often a slight increase in GFR.
-
Sympathetic Nervous System Activity: During periods of stress or low blood pressure, the sympathetic nervous system can constrict both afferent and efferent arterioles, reducing GHP and GFR to conserve blood volume.
Consequences of Glomerular Hydrostatic Pressure Dysregulation
Abnormal GHP can have significant consequences on renal function and overall health.
1. Glomerulonephritis
Inflammatory conditions affecting the glomeruli, such as glomerulonephritis, can damage the glomerular capillaries, altering GHP and causing proteinuria (protein in urine) and hematuria (blood in urine). The increased permeability of the damaged glomeruli leads to a higher than normal GFR initially. However, this is quickly followed by a decline in GFR due to decreased filtering surface area.
2. Hypertension
Sustained hypertension elevates GHP, potentially causing damage to the glomeruli over time. This can lead to glomerulosclerosis, scarring of the glomeruli, and ultimately, chronic kidney disease.
3. Dehydration
Dehydration reduces blood volume, leading to lower GHP and reduced GFR. This triggers the renin-angiotensin-aldosterone system (RAAS) to increase blood volume and maintain blood pressure.
4. Heart Failure
Heart failure reduces cardiac output, decreasing blood pressure and, consequently, GHP. This leads to decreased GFR and potential fluid retention.
5. Renal Failure
Any significant and persistent disruption to GHP, regardless of the cause, can ultimately lead to renal failure, a condition requiring dialysis or kidney transplant for survival.
Conclusion
Glomerular hydrostatic pressure is a cornerstone of renal function. Its precise regulation is essential for maintaining the delicate balance of fluid and electrolyte homeostasis. Understanding the factors influencing GHP and the consequences of its dysregulation is paramount in diagnosing and managing various renal and cardiovascular conditions. Further research into the intricate mechanisms controlling GHP continues to refine our understanding of kidney function and opens avenues for better treatment and prevention of renal diseases. The ongoing investigation into the complex interplay of systemic blood pressure, hormonal influences, and the intrinsic autoregulatory mechanisms of the kidney provides a continuous refinement of our understanding of this vital physiological process. Furthermore, advances in imaging techniques and biomarker analysis are enhancing our ability to detect and monitor changes in GHP, improving early diagnosis and interventions for kidney diseases. This ever-evolving field promises continued improvements in the management and treatment of renal conditions.
Latest Posts
Latest Posts
-
What Is The Lcm Of 2 And 11
Mar 28, 2025
-
In The Burning Of Methane What Are The Reactants
Mar 28, 2025
-
What Is The Difference Between Methanol And Ethanol Fuels
Mar 28, 2025
-
If A Circle Is One How Many Is An Octagon
Mar 28, 2025
-
The Electrons Present In The Outermost Shell Are Called
Mar 28, 2025
Related Post
Thank you for visiting our website which covers about Glomerular Hydrostatic Pressure Is The Pressure Of . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
