What Is The Function Of The Collecting Duct
Juapaving
Apr 01, 2025 · 5 min read
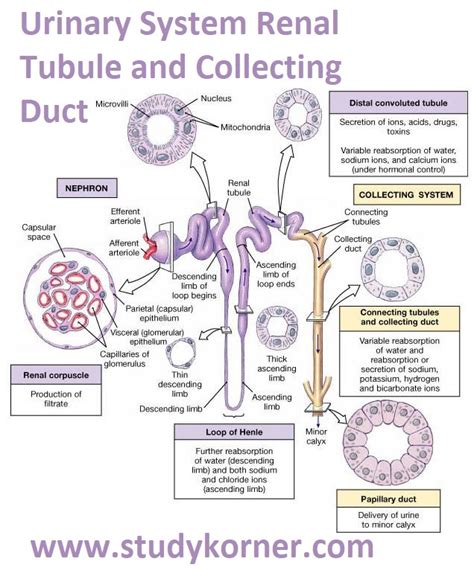
Table of Contents
What is the Function of the Collecting Duct? A Deep Dive into Renal Physiology
The collecting duct, a vital component of the nephron, the functional unit of the kidney, plays a crucial role in regulating fluid balance, electrolyte homeostasis, and blood pressure. Understanding its function is essential to grasping the complexities of renal physiology and its impact on overall health. This article will delve into the intricate mechanisms of the collecting duct, exploring its multifaceted roles in urine concentration, acid-base balance, and potassium regulation.
The Anatomy and Organization of the Collecting Duct System
Before diving into the functions, let's briefly review the anatomy. The collecting duct system is a series of interconnected tubules that receive filtrate from multiple nephrons. It begins with the connecting tubule, which transitions into the cortical collecting duct (CCD) in the renal cortex. The CCD then merges with other collecting ducts to form medullary collecting ducts (MCD), which descend into the renal medulla, deepening into the inner medulla. Finally, several medullary collecting ducts converge to form the papillary duct, emptying urine into a minor calyx.
This structured organization is crucial for the collecting duct's ability to perform its complex functions. The arrangement within the renal medulla, a region with a high concentration gradient, is essential for the creation of concentrated urine.
Water Reabsorption: The Key Role of Antidiuretic Hormone (ADH)
One of the most critical functions of the collecting duct is the regulation of water reabsorption. This process is tightly controlled by antidiuretic hormone (ADH), also known as vasopressin. ADH, released from the posterior pituitary gland in response to increased plasma osmolality (high blood solute concentration) or decreased blood volume, binds to receptors (V2 receptors) on principal cells in the collecting duct.
The Mechanism of ADH-Induced Water Reabsorption
This binding triggers a cascade of intracellular events leading to the insertion of aquaporin-2 (AQP2) water channels into the apical membrane of principal cells. These channels facilitate the movement of water from the tubular lumen (urine) into the interstitial fluid of the medulla. The medullary interstitial fluid possesses a high osmotic concentration, created by the countercurrent multiplication system in the loop of Henle. This osmotic gradient drives the passive reabsorption of water, ultimately concentrating the urine.
Without ADH, AQP2 channels are withdrawn from the apical membrane, reducing water permeability and leading to the excretion of dilute urine. This precise regulation of water reabsorption is critical for maintaining plasma osmolality and blood volume within a narrow physiological range. Diabetes insipidus, a condition characterized by insufficient ADH production or action, exemplifies the consequence of impaired collecting duct water reabsorption, resulting in the production of large volumes of dilute urine.
Electrolyte Regulation: Sodium, Potassium, and Acid-Base Balance
Beyond water reabsorption, the collecting duct is actively involved in regulating electrolyte balance, particularly sodium (Na+), potassium (K+), and hydrogen (H+) ions. These processes are crucial for maintaining proper neuromuscular function, acid-base balance, and overall cellular health.
Sodium Reabsorption: The Role of ENaC Channels
Principal cells in the collecting duct reabsorb sodium through epithelial sodium channels (ENaCs) located in the apical membrane. This sodium reabsorption is driven by the electrochemical gradient and is crucial for regulating blood pressure. Aldosterone, a steroid hormone produced by the adrenal cortex, stimulates ENaC expression and activity, increasing sodium reabsorption. This effect is further amplified by the sodium-potassium ATPase pump on the basolateral membrane, which actively transports sodium out of the cell, maintaining the electrochemical gradient.
Potassium Secretion: A Balancing Act
The collecting duct plays a critical role in potassium homeostasis. Potassium secretion occurs primarily in the principal cells via ROMK channels in the apical membrane. The secretion is influenced by several factors, including potassium intake, aldosterone levels, and acid-base balance. Increased potassium intake or aldosterone levels stimulate potassium secretion, preventing hyperkalemia (high blood potassium).
Acid-Base Balance: The Role of Intercalated Cells
The intercalated cells of the collecting duct are responsible for regulating acid-base balance. These cells have two subtypes: α-intercalated cells and β-intercalated cells. α-intercalated cells secrete protons (H+) into the tubular lumen, contributing to the excretion of acid, while β-intercalated cells secrete bicarbonate (HCO3-) into the tubular lumen, which helps in the excretion of base. This acid-base regulation is critical in maintaining blood pH within the narrow physiological range.
The Impact of Other Hormones and Factors
The function of the collecting duct is not solely dependent on ADH, aldosterone, and the inherent activity of its cells. Several other factors modulate its activity:
-
Atrial Natriuretic Peptide (ANP): Released by the atria in response to increased blood volume, ANP inhibits sodium reabsorption in the collecting duct, promoting sodium and water excretion. This contributes to lowering blood pressure.
-
Prostaglandins: These lipid mediators can influence sodium and water reabsorption, often counteracting the effects of ADH and aldosterone.
-
Parathyroid Hormone (PTH): PTH indirectly influences the collecting duct by modulating calcium reabsorption in the distal convoluted tubule and loop of Henle, indirectly affecting the overall electrolyte balance.
Clinical Significance of Collecting Duct Dysfunction
Disruptions in the function of the collecting duct can lead to several clinical conditions:
-
Diabetes Insipidus: As previously mentioned, impaired ADH action or production results in excessive water loss and dilute urine.
-
Syndrome of Inappropriate Antidiuretic Hormone (SIADH): Excessive ADH secretion causes water retention, hyponatremia (low blood sodium), and concentrated urine.
-
Electrolyte Imbalances: Dysfunction in sodium, potassium, or acid-base regulation can lead to serious consequences, such as cardiac arrhythmias (due to potassium imbalance), and neurological symptoms (due to sodium imbalance).
-
Renal Tubular Acidosis: Impaired acid excretion due to dysfunctional intercalated cells causes metabolic acidosis.
Conclusion: The Collecting Duct's Crucial Role in Renal Physiology
The collecting duct is far more than a simple conduit for urine. It’s a highly regulated structure with a multifaceted role in maintaining fluid and electrolyte balance, blood pressure, and acid-base homeostasis. Its intricate mechanisms, involving hormonal regulation, channel activity, and cellular interactions, demonstrate the remarkable complexity of renal physiology. Understanding the function of the collecting duct is crucial for diagnosing and treating various renal and systemic disorders. Further research into the intricate details of its function continues to provide valuable insights into human physiology and potential therapeutic targets.
Latest Posts
Latest Posts
-
What Are The Vertical Rows On The Periodic Table Called
Apr 02, 2025
-
What Do You Call The Place Where An Organism Lives
Apr 02, 2025
-
What Are The Common Multiples Of 6 And 9
Apr 02, 2025
-
Are Angiosperms Gametophyte Or Sporophyte Dominant
Apr 02, 2025
-
How Many Centimeters Are In 14 Inches
Apr 02, 2025
Related Post
Thank you for visiting our website which covers about What Is The Function Of The Collecting Duct . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
