What Hormone Is The Primary Antagonist Of Glucagon
Juapaving
Mar 19, 2025 · 7 min read
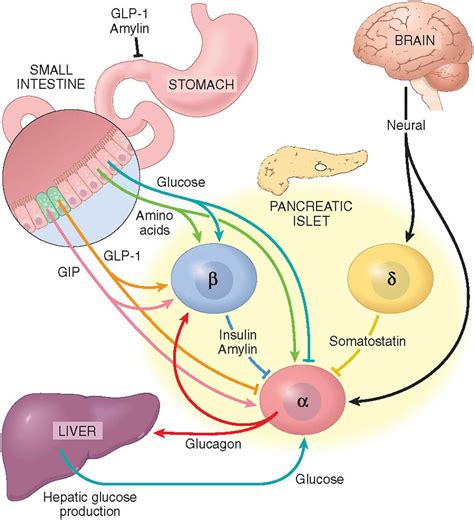
Table of Contents
What Hormone is the Primary Antagonist of Glucagon?
Glucagon, a critical hormone in glucose homeostasis, plays a vital role in regulating blood sugar levels. Its primary function is to increase glucose levels in the blood when they fall too low. But what about the opposing force? What hormone acts as the primary antagonist to glucagon's actions? The answer is insulin. This article will delve deep into the intricacies of the glucagon-insulin relationship, exploring their contrasting roles, mechanisms of action, and the critical implications of their balanced interplay for overall health.
Understanding Glucagon: The Blood Sugar Elevator
Glucagon, secreted by the alpha cells of the pancreas, is a peptide hormone primarily involved in counteracting hypoglycemia (low blood sugar). When blood glucose levels drop, glucagon is released into the bloodstream, triggering a cascade of events designed to raise blood sugar back to normal levels. These actions include:
Glucagon's Key Actions:
- Glycogenolysis: Glucagon stimulates the breakdown of glycogen (stored glucose) in the liver into glucose, which is then released into the bloodstream. This is a rapid process, providing an immediate source of glucose.
- Gluconeogenesis: In the liver and kidneys, glucagon promotes the synthesis of glucose from non-carbohydrate sources like amino acids and glycerol. This is a slower process but provides a sustained source of glucose.
- Ketogenesis: During prolonged fasting or starvation, glucagon stimulates the liver to produce ketone bodies, an alternative energy source for the brain and other tissues when glucose is scarce.
- Inhibition of Glucose Uptake: Glucagon reduces glucose uptake by peripheral tissues, ensuring that available glucose is prioritized for vital organs like the brain.
These actions demonstrate glucagon's crucial role in preventing dangerously low blood sugar levels, a condition that can lead to serious neurological consequences.
Insulin: The Blood Sugar Regulator and Glucagon's Antagonist
Insulin, secreted by the beta cells of the pancreas, is the primary hormone responsible for lowering blood glucose levels. It's the counterbalance to glucagon, working to maintain glucose homeostasis within a narrow, healthy range. Its actions are largely the opposite of glucagon's:
Insulin's Key Actions:
- Glycogenesis: Insulin stimulates the synthesis of glycogen from glucose in the liver and muscles, storing excess glucose for later use.
- Glycolysis and Lipogenesis: Insulin promotes glucose uptake by cells, especially muscle and fat cells. Once inside the cells, glucose is either used for energy through glycolysis or converted into fatty acids and stored as triglycerides in adipose tissue.
- Protein Synthesis: Insulin enhances protein synthesis, using amino acids absorbed from the diet or released from muscle protein breakdown.
- Inhibition of Gluconeogenesis and Ketogenesis: Insulin suppresses gluconeogenesis and ketogenesis, preventing the unnecessary production of glucose and ketone bodies when blood glucose levels are already adequate.
This intricate system of actions ensures that glucose is efficiently utilized for energy, stored for future needs, and that blood sugar levels remain within a tight physiological range.
The Glucagon-Insulin Axis: A Delicate Balance
The relationship between glucagon and insulin is a dynamic and intricate interplay, essential for maintaining glucose homeostasis. They act as reciprocal regulators, responding to changes in blood glucose levels to keep them within a tight range. This finely tuned balance is crucial for health, and disruptions can lead to various metabolic disorders.
The Feedback Loop:
When blood glucose levels rise (e.g., after a meal), insulin secretion increases, while glucagon secretion decreases. This leads to glucose uptake by cells, glycogen synthesis, and reduced glucose production by the liver. Conversely, when blood glucose levels fall (e.g., during fasting or exercise), glucagon secretion increases, while insulin secretion decreases. This triggers glycogenolysis, gluconeogenesis, and reduced glucose uptake, restoring blood glucose levels.
This continuous feedback loop, involving both hormones, is a hallmark of healthy glucose metabolism. It demonstrates the critical antagonistic relationship between glucagon and insulin.
Disruptions in the Glucagon-Insulin Balance: Metabolic Consequences
Imbalances in the glucagon-insulin axis can have significant consequences for health. These imbalances often underlie various metabolic disorders:
Type 1 Diabetes:
In type 1 diabetes, the body's immune system attacks and destroys the insulin-producing beta cells in the pancreas. This leads to a complete lack of insulin, resulting in hyperglycemia (high blood sugar). The absence of insulin's antagonistic effect on glucagon allows for unchecked glucagon activity, further exacerbating hyperglycemia.
Type 2 Diabetes:
Type 2 diabetes is characterized by insulin resistance, where cells become less responsive to insulin's effects. This leads to elevated blood glucose levels despite the pancreas still producing insulin. In many cases, the pancreas attempts to compensate by producing more insulin. Eventually, this compensatory mechanism fails, and beta cells become less efficient, leading to decreased insulin secretion and an increased relative glucagon action. This relative glucagon excess further contributes to hyperglycemia.
Hypoglycemia:
Conversely, excessive insulin secretion or insufficient glucagon secretion can lead to hypoglycemia, a condition characterized by dangerously low blood glucose levels. This can occur in individuals with type 1 or type 2 diabetes who take too much insulin or have impaired glucagon secretion. The lack of counter-regulatory response from glucagon can result in severe symptoms, including seizures and loss of consciousness.
Other Hormones Influencing Glucose Homeostasis: A Broader Perspective
While insulin is the primary antagonist of glucagon, several other hormones play significant, albeit secondary, roles in regulating glucose metabolism. These include:
- Somatostatin: Secreted by the delta cells of the pancreas, somatostatin inhibits both insulin and glucagon secretion, acting as a modulator of the glucagon-insulin axis. It helps to dampen the rapid fluctuations in blood glucose.
- Growth Hormone (GH): GH is an anabolic hormone that promotes growth and development. It can have both insulin-like and insulin-counter-regulatory effects. While it can enhance glucose uptake in some tissues, it also stimulates gluconeogenesis and lipolysis (fat breakdown), thus indirectly influencing blood sugar levels.
- Cortisol: This stress hormone secreted by the adrenal glands has a potent effect on glucose homeostasis. It stimulates gluconeogenesis, raises blood glucose levels, and promotes insulin resistance.
- Epinephrine (Adrenaline): This hormone is released during the "fight-or-flight" response and plays a role in elevating blood glucose levels by stimulating glycogenolysis and gluconeogenesis, similar to glucagon.
- Thyroid Hormones: Thyroid hormones influence metabolic rate. Elevated levels increase glucose turnover, impacting both insulin sensitivity and the overall balance of glucose metabolism.
Understanding the interplay of these hormones provides a comprehensive understanding of the complex regulatory system governing glucose homeostasis.
Maintaining Glucagon-Insulin Balance: Lifestyle Choices Matter
Maintaining a healthy balance between glucagon and insulin is crucial for preventing metabolic disorders. Lifestyle interventions play a key role in this:
- Dietary Choices: A balanced diet, rich in fruits, vegetables, whole grains, and lean protein, helps to regulate blood sugar levels. Limiting refined carbohydrates and sugary drinks is essential.
- Regular Exercise: Regular physical activity improves insulin sensitivity, making cells more responsive to insulin's effects. It also increases glucose uptake by muscles, reducing blood sugar levels.
- Weight Management: Maintaining a healthy weight reduces the risk of insulin resistance and type 2 diabetes.
- Stress Management: Chronic stress can elevate cortisol levels, leading to insulin resistance. Practicing stress-reducing techniques like yoga or meditation can be beneficial.
These lifestyle modifications, along with medical interventions when necessary, contribute significantly to optimizing the delicate balance between glucagon and insulin.
Conclusion: Insulin - The Key Antagonist in Maintaining Glucose Harmony
In conclusion, while other hormones contribute to glucose regulation, insulin stands as the primary antagonist of glucagon. Their coordinated actions, mediated through a complex feedback loop, are essential for maintaining healthy blood sugar levels. Understanding their interplay and the factors affecting this balance is vital for preventing and managing metabolic disorders. By adopting healthy lifestyle choices, individuals can significantly contribute to optimizing their glucagon-insulin axis and safeguarding their metabolic well-being. Maintaining this balance is critical for long-term health and the prevention of conditions like type 1 and type 2 diabetes, as well as hypoglycemia. A comprehensive approach encompassing dietary modifications, regular exercise, stress management, and medical supervision where needed provides the best strategy for achieving and sustaining optimal glucose homeostasis.
Latest Posts
Latest Posts
-
Lcm Of 3 6 And 2
Mar 19, 2025
-
Single Displacement Reaction Examples In Everyday Life
Mar 19, 2025
-
Least Common Multiple Of 14 And 28
Mar 19, 2025
-
What Is The Group Of Dogs Called
Mar 19, 2025
-
Lcm Of 6 4 And 10
Mar 19, 2025
Related Post
Thank you for visiting our website which covers about What Hormone Is The Primary Antagonist Of Glucagon . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
