The Matrix Of Blood Is Called
Juapaving
Mar 09, 2025 · 5 min read
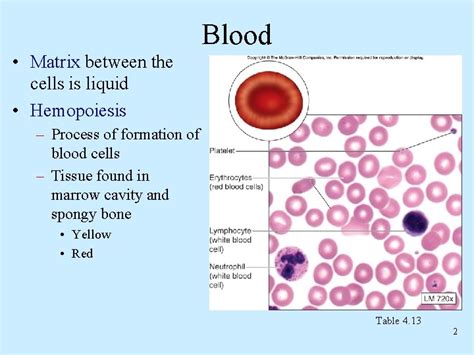
Table of Contents
The Matrix of Blood: Unveiling the Extracellular Matrix and its Crucial Role
The phrase "the matrix of blood" isn't a formally recognized scientific term. Blood itself isn't structured around a traditional extracellular matrix (ECM) in the same way as tissues like bone or cartilage. However, the question highlights the crucial role of the ECM in the overall functionality of the circulatory system and the blood cells themselves. Understanding the complexities of blood, its components, and how they interact necessitates exploring the broader concept of the extracellular matrix and its various influences. This article delves deep into the components of blood, exploring the concepts related to matrix-like structures within and surrounding blood vessels, as well as the ECM's impact on blood cell function and overall vascular health.
Understanding the Extracellular Matrix (ECM)
Before dissecting the intricate relationship between the ECM and blood, it's vital to grasp the fundamental role of the ECM in biological tissues. The extracellular matrix is a complex network of macromolecules—primarily proteins and carbohydrates—that surrounds cells and provides structural and biochemical support. Think of it as the scaffolding upon which tissues are built and maintained. Its composition varies significantly depending on the tissue type.
Key Components of the ECM
- Collagen: The most abundant protein in the ECM, providing tensile strength and structural integrity. Different types of collagen exist, each tailored to specific tissue needs.
- Elastin: Provides elasticity and resilience, allowing tissues to stretch and recoil. Crucial for organs like lungs and blood vessels that experience constant expansion and contraction.
- Proteoglycans: Large molecules composed of a protein core and numerous glycosaminoglycan (GAG) chains. They attract and retain water, contributing to tissue hydration and influencing the mechanical properties of the ECM. They also play vital roles in cell signaling.
- Glycosaminoglycans (GAGs): Long chains of repeating disaccharide units. Their negatively charged nature attracts water and cations, contributing to the compressive strength of the ECM. Examples include hyaluronan, chondroitin sulfate, and heparan sulfate.
- Adhesive glycoproteins: These proteins, such as fibronectin and laminin, mediate cell-matrix interactions. They act as bridges, connecting cells to the ECM and influencing cell adhesion, migration, and differentiation.
The Microenvironment of Blood Vessels: A Specialized ECM
While blood itself doesn't have a typical ECM like connective tissues, the blood vessels that transport blood are embedded within a complex ECM. This perivascular matrix plays a crucial role in vascular homeostasis, influencing vascular tone, blood flow, and the interactions between blood cells and the vascular endothelium (the inner lining of blood vessels).
The Perivascular Matrix: Composition and Function
The perivascular ECM surrounding blood vessels is a dynamic structure composed of a variety of components including:
- Collagen type I and III: Provides structural support and tensile strength to the blood vessel walls.
- Elastin: Allows the blood vessels to stretch and recoil with each heartbeat, ensuring efficient blood flow.
- Proteoglycans and GAGs: Regulate water content and contribute to the mechanical properties of the vessel wall. They also play a key role in the regulation of vascular permeability.
- Adhesive glycoproteins: Facilitate the interaction between vascular cells (endothelial cells, smooth muscle cells) and the ECM, influencing cell adhesion, migration, and signaling.
- Basement membrane: A specialized layer of ECM directly surrounding the endothelial cells, acting as a selective barrier and influencing nutrient transport and cell adhesion.
The composition and organization of the perivascular matrix can significantly influence vascular health. Changes in the ECM composition, such as increased collagen deposition or decreased elastin content, can contribute to vascular stiffness and hypertension. Furthermore, the perivascular matrix provides a structural framework for the recruitment and activation of immune cells in the case of vascular inflammation.
Blood Cells and the ECM: Indirect Interactions
Though blood cells don't directly interact with a classic ECM within the bloodstream, their function and behavior are indirectly influenced by the ECM in several ways.
- Hematopoiesis and the Bone Marrow ECM: Blood cell formation (hematopoiesis) occurs primarily in the bone marrow, a tissue rich in ECM. The bone marrow ECM provides structural support and crucial biochemical signals that regulate the proliferation, differentiation, and maturation of blood cells.
- Interactions with the Endothelial ECM: Blood cells constantly interact with the endothelial cells that line the blood vessels. The endothelial ECM plays a crucial role in regulating blood cell adhesion, trafficking, and activation. For example, during inflammation, endothelial cells undergo changes that alter the ECM composition, allowing immune cells to adhere and migrate out of the bloodstream.
- Thrombosis and the ECM: Blood clotting (thrombosis) is a complex process involving the interaction of platelets, coagulation factors, and the ECM. The ECM components, particularly collagen, play a critical role in platelet activation and fibrin formation, the key components of a blood clot.
The ECM and Vascular Diseases
Dysregulation of the ECM is implicated in various vascular diseases. For example:
- Atherosclerosis: Characterized by the build-up of plaque within the arteries, atherosclerosis involves significant changes in the arterial ECM. Increased collagen deposition and decreased elastin contribute to arterial stiffness, while the accumulation of lipids and inflammatory cells alters the ECM composition further, promoting plaque formation.
- Hypertension: High blood pressure is often associated with alterations in the vascular ECM. Increased collagen deposition and decreased elasticity contribute to vascular stiffening, impairing the ability of blood vessels to accommodate changes in blood flow, thus increasing blood pressure.
- Vascular inflammation: Inflammation of blood vessels is often accompanied by ECM remodeling, with changes in ECM composition and organization influencing the recruitment and activation of immune cells, contributing to the progression of vascular inflammation.
Conclusion: The Indirect Matrix of Blood
While the term "matrix of blood" isn't scientifically precise, the significance of extracellular matrices in the circulatory system is undeniable. The perivascular ECM surrounding blood vessels plays a critical role in maintaining vascular health and integrity. Furthermore, the ECM within the bone marrow is essential for blood cell formation, and ECM interactions influence blood cell behavior throughout the circulatory system. Understanding the composition and function of these matrices is crucial for comprehending the mechanisms of vascular diseases and developing novel therapeutic strategies. Future research focusing on ECM-targeted therapies holds immense promise for treating cardiovascular disorders and improving overall vascular health. The complex interplay between blood, its cells, and the surrounding ECM highlights the interconnectedness of biological systems and the importance of studying these interactions for a comprehensive understanding of health and disease.
Latest Posts
Latest Posts
-
Which Mountain Range Separates Europe From Asia
Mar 09, 2025
-
What Is Oxidized And Reduced In Cellular Respiration
Mar 09, 2025
-
What Is Greater Mb Or Gb
Mar 09, 2025
-
Is Water A Renewable Or A Nonrenewable Resource
Mar 09, 2025
-
Common Factors Of 12 And 9
Mar 09, 2025
Related Post
Thank you for visiting our website which covers about The Matrix Of Blood Is Called . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
