The Kidneys Are Stimulated To Produce Renin
Juapaving
Mar 15, 2025 · 6 min read
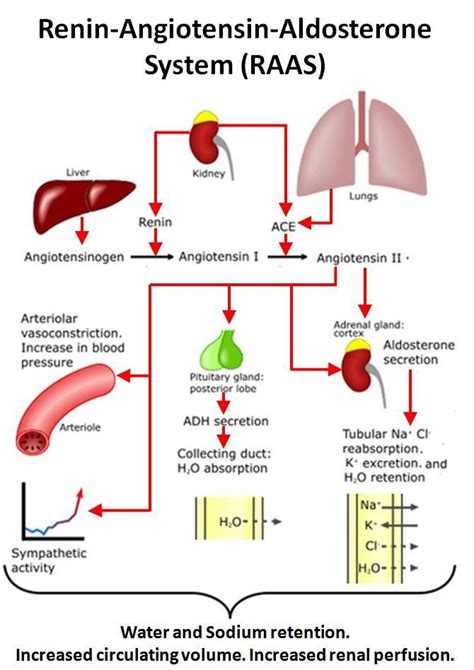
Table of Contents
The Kidneys are Stimulated to Produce Renin: A Deep Dive into the Renin-Angiotensin-Aldosterone System (RAAS)
The kidneys, often overlooked despite their vital role in maintaining bodily homeostasis, play a crucial part in regulating blood pressure through the production of renin. This enzyme, a cornerstone of the Renin-Angiotensin-Aldosterone System (RAAS), is meticulously controlled and released in response to specific stimuli. Understanding these stimuli and the subsequent cascade of events is crucial to comprehending the complexities of blood pressure regulation and various related pathologies. This article will delve into the intricate mechanisms by which the kidneys are stimulated to produce renin, exploring the physiological processes and pathological conditions that influence this critical process.
Understanding the Renin-Angiotensin-Aldosterone System (RAAS)
Before delving into the specific stimuli for renin release, a brief overview of the RAAS is essential. This hormonal system is primarily responsible for regulating blood volume and blood pressure. The process begins with the release of renin from the juxtaglomerular (JG) cells located in the afferent arterioles of the nephrons within the kidneys.
Renin acts on angiotensinogen, a protein produced by the liver, converting it to angiotensin I. Angiotensin I is then further converted to angiotensin II by angiotensin-converting enzyme (ACE), primarily found in the lungs. Angiotensin II, a potent vasoconstrictor, increases blood pressure directly by constricting blood vessels. Furthermore, it stimulates the adrenal cortex to release aldosterone, a hormone that promotes sodium and water reabsorption in the kidneys, ultimately increasing blood volume and further elevating blood pressure.
Key Stimuli for Renin Release: A Detailed Exploration
Several factors trigger the release of renin from the JG cells. These can be broadly categorized into three main mechanisms:
1. Decreased Renal Perfusion Pressure (Intrarenal Baroreceptor Mechanism)
This is arguably the most significant stimulus for renin release. The JG cells act as intrarenal baroreceptors, directly sensing changes in renal blood flow and pressure within the afferent arterioles. A decrease in renal perfusion pressure, indicating reduced blood flow to the kidneys, triggers the release of renin. This is a crucial negative feedback mechanism. Lower blood flow means less blood is filtered by the kidneys, so increasing blood pressure becomes necessary. Renin release, therefore, initiates the RAAS, leading to increased blood volume and pressure to restore renal perfusion.
This mechanism is highly sensitive, responding to even small reductions in renal perfusion pressure. Conditions such as dehydration, hemorrhage, and heart failure can all significantly reduce renal perfusion pressure, thereby stimulating renin release.
2. Sympathetic Nervous System Activation (β1-Adrenergic Stimulation)
The sympathetic nervous system plays a significant role in regulating blood pressure. When blood pressure drops, the sympathetic nervous system is activated, releasing norepinephrine. This neurotransmitter binds to β1-adrenergic receptors located on the JG cells. This stimulation directly promotes renin release, further enhancing the body's attempt to raise blood pressure.
The sympathetic stimulation acts synergistically with the intrarenal baroreceptor mechanism. In situations of low blood pressure, both mechanisms work in concert to trigger renin release, amplifying the overall response.
3. Decreased Sodium Chloride Delivery to the Distal Tubule (Macula Densa Mechanism)
The macula densa, a specialized group of cells located in the distal convoluted tubule, plays a crucial role in regulating renin release. These cells monitor the concentration of sodium chloride in the tubular fluid. A decrease in sodium chloride delivery to the macula densa signals a decrease in overall renal perfusion and triggers renin release.
This mechanism is closely linked to the glomerulotubular balance, which ensures that the amount of sodium and water reabsorbed in the distal tubules is proportional to the glomerular filtration rate. When sodium chloride delivery decreases, it suggests reduced glomerular filtration, thus prompting renin release.
Other Factors Influencing Renin Release
While the three main mechanisms outlined above are the dominant factors, several other factors can modulate renin release:
-
Prostaglandins: Certain prostaglandins, such as PGE2 and PGI2, inhibit renin release. Conversely, inhibition of prostaglandin synthesis can increase renin release.
-
Dopamine: Dopamine, acting on dopaminergic receptors in the JG cells, inhibits renin release.
-
Atrial Natriuretic Peptide (ANP): ANP, released from the atria of the heart in response to increased blood volume, inhibits renin release.
-
Angiotensin II: While angiotensin II is a downstream product of the RAAS, it exhibits negative feedback on renin release. Increased angiotensin II levels inhibit further renin secretion. This negative feedback loop prevents excessive activation of the RAAS and helps maintain blood pressure homeostasis.
Pathological Conditions Affecting Renin Release
Dysregulation of renin release is implicated in several pathological conditions:
-
Hypertension: Overactivation of the RAAS, resulting in excessive renin release, can contribute to hypertension (high blood pressure). This can be due to various factors, including renal artery stenosis (narrowing of the renal arteries), and genetic predisposition.
-
Hypovolemia: Conditions causing decreased blood volume, such as dehydration and hemorrhage, trigger increased renin release as a compensatory mechanism.
-
Heart Failure: In heart failure, reduced cardiac output leads to decreased renal perfusion, stimulating renin release. This, however, exacerbates the condition by further increasing blood volume and cardiac workload.
-
Renal Artery Stenosis: Narrowing of the renal arteries reduces renal perfusion pressure, leading to significant increases in renin release, contributing to secondary hypertension.
-
Primary Aldosteronism (Conn's Syndrome): This condition is characterized by excessive aldosterone secretion by the adrenal glands, often unrelated to RAAS activation. While not directly affecting renin release, it can mask the elevated renin levels that might otherwise be present.
Clinical Significance and Therapeutic Implications
Understanding the mechanisms of renin release has significant clinical implications. Measuring plasma renin activity (PRA) is a valuable diagnostic tool in evaluating various renal and cardiovascular diseases. Furthermore, several drugs target the RAAS to manage hypertension and heart failure. These include:
-
ACE inhibitors: These drugs block ACE, preventing the conversion of angiotensin I to angiotensin II, thereby reducing vasoconstriction and aldosterone release.
-
Angiotensin receptor blockers (ARBs): ARBs block the action of angiotensin II at its receptors, achieving a similar effect to ACE inhibitors.
-
Direct renin inhibitors: These newer drugs directly inhibit renin, preventing the initiation of the RAAS cascade.
Careful monitoring of renin levels and tailoring therapeutic interventions are crucial in managing these conditions effectively.
Conclusion: The Complex Dance of Homeostasis
The kidneys' role in producing renin is integral to maintaining blood pressure and fluid balance within the body. The intricate interplay of factors stimulating renin release reflects the body's complex mechanisms for maintaining homeostasis. Understanding these stimuli and the subsequent cascade of events in the RAAS is fundamental to comprehending various physiological processes and pathophysiological conditions. The development of targeted therapeutic strategies focused on the RAAS underscores the profound clinical significance of the kidneys' role in regulating renin production and, by extension, blood pressure. Further research into the fine-tuning mechanisms of this system promises to yield even greater insights into the prevention and treatment of cardiovascular and renal diseases.
Latest Posts
Latest Posts
-
Determine Charge On Capacitor In Following Circuit
Mar 15, 2025
-
Nouns That Begin With The Letter O
Mar 15, 2025
-
Difference Between A Generator And Alternator
Mar 15, 2025
-
What Is Xix In Roman Numerals
Mar 15, 2025
-
What Is The Least Common Multiple Of 5 And 7
Mar 15, 2025
Related Post
Thank you for visiting our website which covers about The Kidneys Are Stimulated To Produce Renin . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
