The Double-walled Sac Enclosing The Heart Is Called The
Juapaving
Mar 10, 2025 · 7 min read
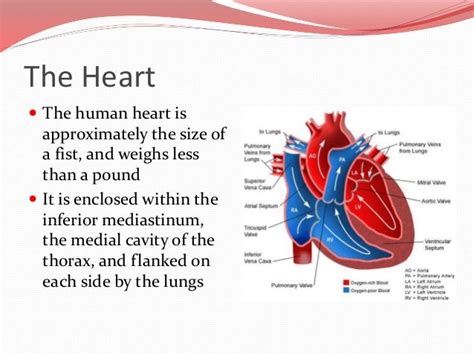
Table of Contents
The Double-Walled Sac Enclosing the Heart: A Deep Dive into the Pericardium
The heart, the tireless engine of our circulatory system, doesn't simply float freely within the chest cavity. It's meticulously cradled and protected by a double-walled sac known as the pericardium. Understanding the pericardium's structure, function, and associated pathologies is crucial for comprehending cardiovascular health and disease. This comprehensive article will explore the intricacies of this vital structure, examining its layers, clinical significance, and the potential consequences of pericardial dysfunction.
Anatomy of the Pericardium: Layers and Structure
The pericardium is a fibroserous sac, meaning it's composed of both fibrous and serous tissue. This layered structure provides both robust protection and a friction-free environment for the heart's rhythmic contractions. Let's dissect its two main components:
1. Fibrous Pericardium: The Outermost Layer
The fibrous pericardium, the outermost layer, is a tough, inelastic, and dense connective tissue sac. Think of it as the heart's strong, protective casing. Its primary functions include:
- Protection: It shields the heart from external trauma and prevents overdistension. Its strong, fibrous nature acts as a barrier against excessive stretching or tearing.
- Anchorage: The fibrous pericardium anchors the heart to surrounding structures, including the diaphragm and the great vessels (aorta, vena cava). This prevents excessive movement and maintains its position within the mediastinum.
- Structural Support: It provides structural support to the heart and prevents the heart chambers from over-expanding during contraction.
2. Serous Pericardium: The Inner Layer—A Delicate Embrace
Nestled within the fibrous pericardium is the serous pericardium, a much more delicate and thinner layer. It's further subdivided into two continuous layers:
- Parietal Pericardium: This layer lines the inner surface of the fibrous pericardium. It's essentially the outer layer of the serous pericardium.
- Visceral Pericardium (Epicardium): This layer is intimately adhered to the heart's surface. It's functionally part of the heart wall itself, forming the outermost layer of the cardiac muscle.
Between the parietal and visceral layers lies the pericardial cavity, a potential space containing a small amount of serous fluid (pericardial fluid). This fluid acts as a lubricant, minimizing friction between the two serous layers during the heart's continuous contractions. This friction reduction is essential for efficient and energy-conserving heart function. Without this lubricating fluid, the constant rubbing would damage the delicate heart muscle.
Functions of the Pericardium: More Than Just a Protective Sac
While its protective function is paramount, the pericardium plays other crucial roles in maintaining cardiovascular health:
- Preventing Overdistension: The fibrous pericardium's inelasticity prevents excessive expansion of the heart chambers, safeguarding against potentially damaging overfilling. This is particularly crucial during periods of increased venous return or cardiac overload.
- Lubrication and Friction Reduction: The pericardial fluid in the pericardial cavity acts as a lubricant, ensuring smooth movement of the heart within the chest cavity. This friction reduction is essential for efficient and energy-conserving cardiac function.
- Maintaining Cardiac Position: The pericardium helps to anchor the heart in place, preventing excessive movement and maintaining its correct anatomical position within the mediastinum.
- Protecting Against Infection: The pericardium acts as a physical barrier, offering some level of protection against the spread of infection to the heart itself.
Clinical Significance: When the Pericardium Fails
While typically a silent protector, the pericardium can become the site of various pathological conditions. Understanding these conditions is crucial for proper diagnosis and management.
Pericarditis: Inflammation of the Pericardium
Pericarditis refers to inflammation of the pericardium. This condition can arise from a variety of causes, including viral infections, bacterial infections, autoimmune diseases (such as lupus or rheumatoid arthritis), myocardial infarction (heart attack), and even cancer. The inflammation leads to pain, usually sharp and stabbing, often worsened by lying down or deep breathing. In severe cases, a significant buildup of fluid can occur (pericardial effusion), potentially leading to cardiac tamponade.
Pericardial Effusion: Fluid Buildup in the Pericardial Cavity
Pericardial effusion is the accumulation of excessive fluid within the pericardial cavity. This fluid buildup can be caused by a variety of factors, including pericarditis, heart failure, cancer, kidney failure, and certain medications. The fluid can compress the heart, impairing its ability to fill effectively. This condition can range from asymptomatic to life-threatening, depending on the rate and amount of fluid accumulation.
Cardiac Tamponade: A Life-Threatening Emergency
Cardiac tamponade is a life-threatening condition resulting from rapid accumulation of fluid or blood in the pericardial cavity. The pressure from this fluid compresses the heart, hindering its ability to fill with blood and pump effectively. This can lead to a significant drop in blood pressure, shock, and potentially death if not treated promptly. Symptoms include hypotension (low blood pressure), muffled heart sounds, and jugular venous distension. Immediate medical intervention, often involving pericardiocentesis (removal of fluid from the pericardial cavity), is necessary.
Constrictive Pericarditis: Scarring and Restriction
Constrictive pericarditis is a chronic condition characterized by scarring and thickening of the pericardium. This thickening restricts the heart's ability to expand fully during diastole (the relaxation phase of the heart cycle), impairing its filling capacity. The result is decreased cardiac output and symptoms that mimic heart failure. Diagnosis often requires imaging studies and invasive procedures.
Diagnostic Methods: Unveiling Pericardial Secrets
Diagnosing pericardial pathologies requires a multi-faceted approach involving various diagnostic techniques:
- Physical Examination: Auscultation (listening to the heart sounds) can reveal characteristic sounds associated with pericarditis (pericardial friction rub). Examination for signs of reduced cardiac output (low blood pressure, weak pulses) is crucial.
- Electrocardiogram (ECG): The ECG can reveal characteristic changes associated with pericarditis, such as ST-segment elevation or PR-segment depression.
- Chest X-Ray: A chest X-ray can help visualize the size and shape of the heart, as well as the presence of any significant pericardial effusion.
- Echocardiography: Echocardiography (ultrasound of the heart) provides detailed images of the heart and pericardium, allowing visualization of fluid accumulation, thickening of the pericardium, and assessment of heart function.
- Computed Tomography (CT) Scan: CT scans can provide further anatomical detail of the pericardium and surrounding structures.
- Magnetic Resonance Imaging (MRI): MRI offers excellent soft tissue contrast and can be particularly helpful in evaluating the extent and nature of pericardial inflammation and scarring.
Treatment Strategies: Addressing Pericardial Issues
Treatment approaches for pericardial diseases vary depending on the underlying cause and severity of the condition:
- Pericarditis Treatment: Treatment for pericarditis focuses on managing the underlying cause (e.g., treating infection with antibiotics) and relieving symptoms. Nonsteroidal anti-inflammatory drugs (NSAIDs) are often used to reduce inflammation and pain. In severe cases, corticosteroids may be necessary.
- Pericardial Effusion Treatment: Management of pericardial effusion depends on the rate and amount of fluid accumulation and the presence of hemodynamic compromise (impaired blood flow). Pericardiocentesis (draining fluid from the pericardial cavity) is often used to relieve pressure on the heart.
- Cardiac Tamponade Treatment: Cardiac tamponade requires immediate intervention. Pericardiocentesis is the primary treatment to rapidly relieve pressure on the heart and restore cardiac function.
- Constrictive Pericarditis Treatment: Treatment for constrictive pericarditis is often surgical. Pericardiectomy (surgical removal of the pericardium) is often necessary to relieve the restrictive effect on the heart.
Conclusion: The Pericardium—A Vital Unsung Hero
The pericardium, while often overlooked, plays a critical role in maintaining the health and function of the heart. Its double-walled structure provides both protection and a friction-free environment for cardiac contractions. Understanding its anatomy, physiology, and associated pathologies is essential for healthcare professionals and patients alike. Early diagnosis and appropriate management of pericardial diseases are crucial for minimizing complications and improving patient outcomes. The pericardium, although often silent, is a vital component of a healthy cardiovascular system. Its proper function is crucial for the heart's relentless performance, ensuring the continuous circulation that sustains life.
Latest Posts
Latest Posts
-
Whats The Square Root Of 576
Mar 11, 2025
-
A Plasma Protein Essential For Blood Coagulation Is
Mar 11, 2025
-
What Is The Prime Factorization 140
Mar 11, 2025
-
In The Figure What Is The Value Of X
Mar 11, 2025
-
What Is Xxviii In Roman Numerals
Mar 11, 2025
Related Post
Thank you for visiting our website which covers about The Double-walled Sac Enclosing The Heart Is Called The . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
