Functional And Structural Unit Of Kidney
Juapaving
Mar 23, 2025 · 8 min read
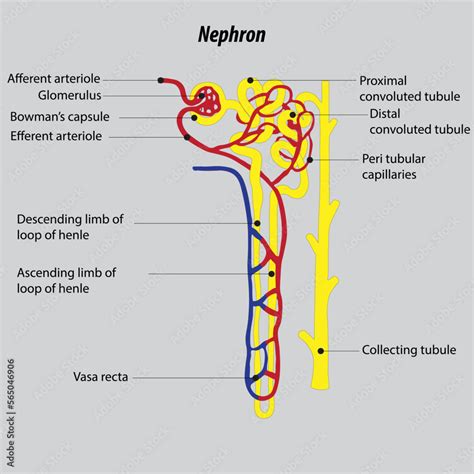
Table of Contents
The Functional and Structural Unit of the Kidney: A Deep Dive into the Nephron
The kidney, a vital organ in the urinary system, plays a crucial role in maintaining homeostasis within the body. Its primary functions include filtering blood, regulating blood pressure, controlling electrolyte balance, and producing hormones like erythropoietin and renin. Understanding how the kidney performs these complex tasks requires a deep dive into its fundamental structural and functional unit: the nephron. This article will explore the intricate structure of the nephron, its complex functions, and how its components work together to ensure efficient kidney function.
The Nephron: The Workhorse of the Kidney
The nephron is the functional unit of the kidney. Each kidney contains approximately one million nephrons, and their combined activity determines the overall efficiency of the kidney. These microscopic structures are responsible for filtering blood, reabsorbing essential substances, and excreting waste products. The nephron's efficiency is vital for maintaining bodily fluid balance and overall health. Damage to nephrons, often through disease or injury, significantly impairs kidney function.
Structure of the Nephron: A Detailed Examination
The nephron is composed of two main parts: the renal corpuscle and the renal tubule.
1. Renal Corpuscle: The Filtration Site
The renal corpuscle, also known as the Malpighian corpuscle, is the initial filtering unit of the nephron. It consists of two structures:
-
Glomerulus: A network of capillaries where blood filtration occurs. The glomerulus is specialized; its capillaries are fenestrated, meaning they have pores that allow for efficient filtration. The pressure within the glomerulus drives the filtration process. The glomerular filtration rate (GFR) is a crucial indicator of kidney health, reflecting the volume of blood filtered per unit of time. A reduced GFR signifies impaired kidney function.
-
Bowman's Capsule: A double-walled cup-shaped structure surrounding the glomerulus. It collects the filtrate produced by the glomerulus, initiating its journey through the renal tubule. The filtrate consists of water, small molecules like glucose and amino acids, ions, and waste products. Larger molecules, such as proteins and blood cells, are typically excluded from the filtrate due to the selective permeability of the glomerular capillaries and Bowman's capsule.
2. Renal Tubule: Reabsorption and Secretion
The renal tubule is a long, convoluted structure extending from Bowman's capsule. It's divided into several segments, each with specialized functions in reabsorbing essential substances and secreting unwanted ones:
-
Proximal Convoluted Tubule (PCT): This segment is responsible for the majority of reabsorption in the nephron. Nutrients like glucose, amino acids, and vitamins are actively reabsorbed back into the bloodstream. A significant amount of water and ions (sodium, potassium, chloride, bicarbonate) are also reabsorbed passively or through active transport mechanisms. The PCT also plays a role in secreting certain substances, such as hydrogen ions and drugs, into the filtrate. Impairment of the PCT significantly affects the body's ability to retain essential nutrients and manage its acid-base balance.
-
Loop of Henle: This U-shaped structure extends deep into the renal medulla. Its unique anatomy creates a concentration gradient within the medulla, crucial for concentrating urine. The descending limb is highly permeable to water but less permeable to ions. The ascending limb is impermeable to water but actively transports ions, particularly sodium, out of the filtrate and into the medullary interstitium. This countercurrent mechanism significantly contributes to water reabsorption and the formation of concentrated urine. Dysfunction of the loop of Henle can lead to the production of dilute urine and electrolyte imbalances.
-
Distal Convoluted Tubule (DCT): This segment is shorter than the PCT and plays a critical role in fine-tuning the composition of the filtrate. It regulates the reabsorption of sodium and calcium ions under the influence of hormones like aldosterone and parathyroid hormone. It also secretes potassium and hydrogen ions, contributing to electrolyte and acid-base balance. The DCT's role in precise control highlights the intricate regulatory mechanisms that maintain homeostasis.
-
Collecting Duct: Multiple distal convoluted tubules converge into a single collecting duct. These ducts run through the medulla and are crucial in regulating water reabsorption, responding to the antidiuretic hormone (ADH). ADH increases the permeability of the collecting duct to water, allowing for greater water reabsorption and the production of more concentrated urine. The collecting duct is also involved in acid-base balance through the secretion of hydrogen ions. Proper functioning of the collecting duct is vital for maintaining water balance and preventing dehydration or overhydration.
Nephron Function: A Detailed Look at the Processes
The nephron's function is complex, involving three main processes: glomerular filtration, tubular reabsorption, and tubular secretion.
1. Glomerular Filtration: The Initial Filtering Process
Glomerular filtration is the first step in urine formation. Driven by blood pressure, water and small dissolved substances move from the glomerular capillaries into Bowman's capsule. The filtration process is highly efficient, with approximately 180 liters of filtrate produced daily. The filtration membrane, composed of the fenestrated capillaries, glomerular basement membrane, and podocytes, acts as a selective barrier, preventing the passage of larger molecules like proteins and blood cells. Any significant alteration in glomerular filtration rate (GFR) may indicate underlying kidney problems.
2. Tubular Reabsorption: Reclaiming Essential Substances
Tubular reabsorption involves the selective reabsorption of essential substances from the filtrate back into the bloodstream. This process occurs mainly in the PCT, Loop of Henle, and DCT. Nutrients like glucose, amino acids, and vitamins are completely reabsorbed in a healthy kidney. Water and ions are also reabsorbed in varying degrees, depending on the body's fluid and electrolyte balance. Hormones like aldosterone and ADH play vital roles in regulating reabsorption. Defective reabsorption mechanisms can result in nutrient loss and electrolyte disturbances.
3. Tubular Secretion: Eliminating Unwanted Substances
Tubular secretion is the process of actively transporting substances from the peritubular capillaries into the filtrate. This process complements glomerular filtration by selectively removing unwanted substances from the blood that were not filtered initially. Hydrogen ions, potassium ions, and certain drugs are actively secreted into the filtrate. This helps in maintaining acid-base balance, regulating potassium levels, and eliminating toxins. Dysfunction in tubular secretion can impair the body's ability to manage acid-base balance and remove toxins.
Juxtamedullary and Cortical Nephrons: Two Types, Different Roles
Nephrons are categorized into two types based on their location and structure: cortical nephrons and juxtamedullary nephrons.
Cortical Nephrons: The Majority
Cortical nephrons are the more numerous type, located primarily in the cortex of the kidney. They have shorter loops of Henle that extend only slightly into the medulla. They play a significant role in filtering blood and reabsorbing essential substances.
Juxtamedullary Nephrons: Concentrating Urine
Juxtamedullary nephrons have long loops of Henle that extend deep into the renal medulla. Their long loops are crucial for establishing the medullary concentration gradient, enabling the kidneys to produce concentrated urine. This ability is vital for conserving water, especially in conditions of dehydration.
The Juxtaglomerular Apparatus: Regulation of Blood Pressure and GFR
The juxtaglomerular apparatus (JGA) is a specialized structure located where the distal convoluted tubule comes into contact with the afferent and efferent arterioles of the glomerulus. It plays a crucial role in regulating blood pressure and glomerular filtration rate (GFR).
The JGA consists of:
-
Juxtaglomerular cells: Specialized smooth muscle cells in the afferent arteriole that secrete renin, an enzyme involved in the renin-angiotensin-aldosterone system (RAAS). The RAAS is vital for regulating blood pressure.
-
Macula densa: Specialized cells in the distal convoluted tubule that monitor the sodium concentration in the filtrate. They signal the juxtaglomerular cells to adjust renin secretion, influencing blood pressure and GFR.
Clinical Significance: Kidney Disease and Nephron Damage
Nephron damage can significantly impact kidney function and overall health. Numerous diseases and conditions can lead to nephron dysfunction, including:
-
Glomerulonephritis: Inflammation of the glomeruli, often due to immune system disorders.
-
Diabetic nephropathy: Kidney damage caused by diabetes, leading to reduced GFR.
-
Hypertensive nephropathy: Kidney damage due to high blood pressure.
-
Polycystic kidney disease: A genetic disorder causing the growth of cysts in the kidneys.
These conditions often lead to chronic kidney disease (CKD), characterized by progressive loss of nephron function. Early detection and management are vital to slow the progression of CKD and improve patient outcomes. Understanding the nephron’s structure and function is crucial for diagnosis, treatment, and management of kidney diseases.
Conclusion: The Intricate Machinery of Renal Function
The nephron, the structural and functional unit of the kidney, is a remarkably complex structure performing a multitude of vital functions essential for maintaining homeostasis. Its intricate architecture and finely tuned processes enable the kidneys to filter blood, regulate blood pressure, control electrolyte balance, and produce essential hormones. Understanding the intricate workings of the nephron provides invaluable insights into kidney physiology and the pathophysiology of kidney diseases. Furthermore, appreciating the complexity of this microscopic unit highlights the remarkable ability of the human body to maintain a stable internal environment despite external variations and challenges. The detailed study of the nephron remains a cornerstone of renal physiology and is essential for advancing our understanding and treatment of kidney disease.
Latest Posts
Latest Posts
-
5 Letter Words Beginning With Pra
Mar 25, 2025
-
Alternation Of Generations Means That Plants Produce
Mar 25, 2025
-
What Is The Factors Of 225
Mar 25, 2025
-
What Does Lv Mean In Roman Numerals
Mar 25, 2025
-
How Are Cellular Respiration And Photosynthesis Interrelated
Mar 25, 2025
Related Post
Thank you for visiting our website which covers about Functional And Structural Unit Of Kidney . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
