Cells That Are Produced By The Testes And Ovaries
Juapaving
Mar 25, 2025 · 6 min read
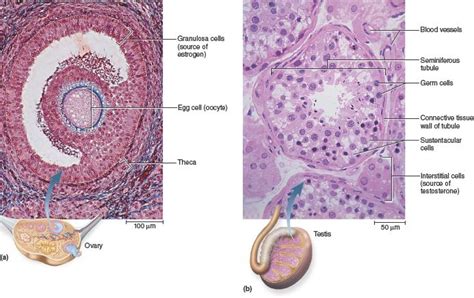
Table of Contents
Cells Produced by the Testes and Ovaries: A Deep Dive into Gametogenesis and Steroidogenesis
The testes and ovaries, the primary reproductive organs in males and females respectively, are responsible for producing gametes (sex cells) and hormones crucial for sexual development and reproduction. Understanding the cellular processes within these organs is fundamental to comprehending human reproductive biology. This article will delve into the various cell types produced by the testes and ovaries, exploring their roles, functions, and the intricate processes that govern their development.
The Testes: A Factory for Sperm and Hormones
The testes, housed within the scrotum, are responsible for spermatogenesis, the process of sperm production, and the synthesis of male sex hormones, primarily testosterone. This dual function necessitates a diverse population of cells working in concert.
1. Germ Cells: The Sperm Precursors
Spermatogenesis begins with spermatogonial stem cells (SSCs), located in the seminiferous tubules. These self-renewing cells are responsible for maintaining the pool of germ cells throughout a male's reproductive life. Through a process of mitosis, SSCs give rise to type A spermatogonia and type B spermatogonia. Type A spermatogonia maintain the SSC pool, while type B spermatogonia are committed to differentiation into mature sperm.
Type B spermatogonia undergo several rounds of mitotic divisions, transforming into primary spermatocytes. These cells then undergo meiosis I, a reductional division that halves the chromosome number, resulting in secondary spermatocytes. Meiosis II, an equational division, follows, producing haploid spermatids.
Spermatids are not yet functional sperm. They undergo a complex process called spermiogenesis, a series of morphological changes that transform them into mature, motile spermatozoa. These changes include the formation of the acrosome (a cap-like structure containing enzymes crucial for fertilization), the condensation of the nucleus, the development of a flagellum (tail), and the shedding of excess cytoplasm.
The entire process of spermatogenesis, from SSC to mature spermatozoa, takes approximately 70 days. It's a highly regulated and coordinated process, dependent on various supporting cells within the seminiferous tubules.
2. Somatic Cells: The Supporting Cast
Several somatic cell types are essential for supporting spermatogenesis within the seminiferous tubules. These include:
-
Sertoli cells: These are elongated cells that form the structural framework of the seminiferous tubules. They provide physical support, nutrition, and hormonal regulation to developing germ cells. Sertoli cells secrete inhibin, a hormone that regulates FSH production, and anti-Müllerian hormone (AMH), crucial during embryonic development. They also form the blood-testis barrier, which protects developing germ cells from the immune system.
-
Leydig cells: Located in the interstitial tissue surrounding the seminiferous tubules, Leydig cells are responsible for producing testosterone. This hormone is crucial for the development and maintenance of secondary sexual characteristics, spermatogenesis, and libido. Leydig cell function is regulated by the luteinizing hormone (LH) from the anterior pituitary gland.
The intricate interplay between germ cells and somatic cells within the seminiferous tubules ensures the continuous production of mature, functional sperm.
The Ovaries: Orchestrating Oogenesis and Hormone Production
The ovaries, located in the pelvic cavity, are responsible for oogenesis, the process of egg production, and the synthesis of female sex hormones, including estrogen and progesterone. Like the testes, the ovaries contain a diverse array of cell types.
1. Germ Cells: The Egg Precursors
Oogenesis begins during fetal development with the formation of oogonia, which undergo mitotic divisions to produce a large pool of primary oocytes. These primary oocytes enter meiosis I but arrest in prophase I until puberty.
At puberty, under the influence of follicle-stimulating hormone (FSH), a small number of primary oocytes resume meiosis I, completing the first meiotic division and producing a secondary oocyte and a first polar body. The secondary oocyte then proceeds to meiosis II, but arrests in metaphase II unless fertilization occurs. If fertilization occurs, meiosis II is completed, producing a mature ovum and a second polar body. The polar bodies are essentially discarded, ensuring that the majority of the cytoplasm goes to the ovum.
Unlike spermatogenesis, which produces millions of sperm throughout a male's lifetime, oogenesis is a finite process. A female is born with a finite number of primary oocytes, and the number decreases throughout her life.
2. Somatic Cells: The Follicular Framework
The development of oocytes within the ovary is intimately linked to the ovarian follicles. These follicles are composed of various somatic cells, including:
-
Granulosa cells: These cells surround the oocyte, forming layers that increase in number as the follicle matures. They secrete estrogen and other factors that support oocyte growth and maturation. They are crucial for the development of the corpus luteum after ovulation.
-
Theca cells: Located outside the granulosa cells, theca cells produce androgens (like androstenedione) which are converted to estrogen by the granulosa cells under the influence of FSH. LH stimulates theca cell androgen production.
-
Cumulus cells: A specialized group of granulosa cells that surround the oocyte immediately before ovulation. They provide crucial support and communication with the oocyte.
As the follicle matures, it undergoes several stages: primordial follicle, primary follicle, secondary follicle, and Graafian follicle (mature follicle). The Graafian follicle ruptures during ovulation, releasing the secondary oocyte into the fallopian tube.
3. Post-Ovulatory Structures
After ovulation, the remaining follicular cells transform into the corpus luteum. This temporary endocrine gland secretes progesterone and estrogen, preparing the uterus for potential pregnancy. If fertilization does not occur, the corpus luteum degenerates, and its hormone production ceases. If pregnancy occurs, the corpus luteum is maintained by human chorionic gonadotropin (hCG) produced by the developing embryo, ensuring continued hormone production for pregnancy maintenance.
The Hormonal Symphony: Interplay between Testes, Ovaries, and Pituitary Gland
The production of gametes and sex hormones is intricately regulated by the hypothalamic-pituitary-gonadal (HPG) axis. The hypothalamus secretes gonadotropin-releasing hormone (GnRH), which stimulates the anterior pituitary gland to release FSH and LH. These gonadotropins act on the testes and ovaries, stimulating gametogenesis and steroidogenesis. The hormones produced by the gonads (testosterone, estrogen, progesterone, inhibin) then exert negative feedback on the hypothalamus and pituitary gland, regulating hormone production. This feedback loop ensures that hormone levels are maintained within a physiological range.
Clinical Significance: Disorders of Gametogenesis and Steroidogenesis
Disruptions in the production of cells by the testes and ovaries can lead to various reproductive disorders. These include:
- Infertility: Impaired spermatogenesis or oogenesis can result in infertility.
- Hypogonadism: Reduced production of sex hormones can lead to hypogonadism, characterized by delayed puberty, reduced libido, and decreased fertility.
- Polycystic ovary syndrome (PCOS): A hormonal disorder affecting women, characterized by ovarian cysts, irregular periods, and hormonal imbalances.
- Testicular cancer: Cancer of the testes can disrupt spermatogenesis and hormone production.
- Ovarian cancer: Cancer of the ovaries can impair oogenesis and hormone production.
Conclusion
The testes and ovaries are remarkable organs, housing a complex array of cells that work in concert to produce gametes and sex hormones essential for reproduction. The intricate processes of spermatogenesis and oogenesis, governed by hormonal regulation and cellular interactions, are fundamental to human reproductive biology. Understanding these processes is crucial not only for comprehending normal reproductive function but also for diagnosing and treating various reproductive disorders. Further research continues to unveil the complexities of these vital organs and their role in human health. Continued study will undoubtedly lead to advancements in reproductive medicine and improve the lives of individuals struggling with infertility or other reproductive issues.
Latest Posts
Latest Posts
-
Word That Starts With A V
Mar 26, 2025
-
The Red Data Book Keeps A Record Of All The
Mar 26, 2025
-
What Are The Inner Transition Metals
Mar 26, 2025
-
How Many Liters Is 6 Gallons
Mar 26, 2025
-
A Group Of Fish Is Called A
Mar 26, 2025
Related Post
Thank you for visiting our website which covers about Cells That Are Produced By The Testes And Ovaries . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
