What Prevents The Trachea From Collapsing
Juapaving
Mar 04, 2025 · 5 min read
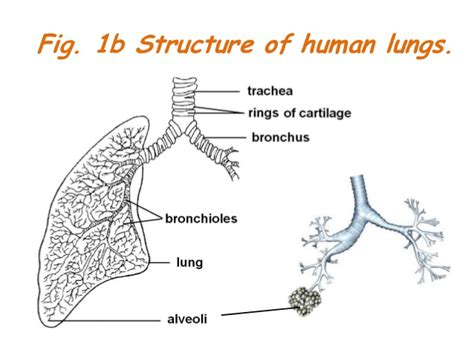
Table of Contents
What Prevents the Trachea from Collapsing? A Deep Dive into Structural Integrity and Respiratory Mechanics
The trachea, or windpipe, is a vital component of the respiratory system, responsible for conducting air to and from the lungs. Its crucial role necessitates a robust structure capable of withstanding the pressures and forces involved in breathing. But what precisely prevents this flexible tube from collapsing, particularly during the forceful exhalations and changes in intrathoracic pressure we experience daily? This article explores the intricate interplay of anatomical features, biomechanical properties, and physiological mechanisms that ensure the trachea remains patent – open and unobstructed – allowing for efficient respiration.
The Structural Pillars of Tracheal Patency
The trachea's ability to remain open despite significant internal and external forces relies heavily on its unique anatomical design. Several key features contribute to its structural integrity:
1. Cartilaginous Rings: The Foundation of Support
The most prominent feature providing tracheal support is the series of C-shaped hyaline cartilage rings. These rings, typically 16 to 20 in number, are not complete circles; instead, they are open posteriorly, forming a horseshoe shape. This incomplete ring design is crucial for several reasons:
-
Flexibility: The posterior gap allows for flexibility during swallowing. The esophagus, the tube carrying food to the stomach, lies directly behind the trachea. The open-ended cartilage allows the trachea to compress slightly to make way for food boluses, preventing choking.
-
Controlled Expansion and Contraction: The posterior membrane, composed of smooth muscle and connective tissue, is capable of controlled expansion and contraction. This allows for adjustments in tracheal diameter during respiration, accommodating changes in airflow and lung volume.
-
Strength and Rigidity: The hyaline cartilage itself provides significant rigidity, resisting the inward collapse of the tracheal lumen (the inner space) under negative intrathoracic pressure. This is particularly important during inspiration when the pressure within the chest cavity becomes lower than atmospheric pressure.
2. Trachealis Muscle: Fine-Tuning Tracheal Diameter
The posterior gap in the cartilage rings is bridged by the trachealis muscle. This smooth muscle plays a vital role in:
-
Coughing and Expulsive Forces: During forceful exhalations, such as coughing, the trachealis muscle contracts, constricting the tracheal diameter. This increases the velocity of airflow, facilitating the expulsion of irritants or mucus.
-
Regulation of Airflow: Although less prominent than its role in coughing, the trachealis muscle participates in fine-tuning tracheal diameter during normal breathing, helping to regulate airflow resistance.
-
Protection against Collapse: While not the primary structural support, the trachealis muscle contributes to the overall stability of the trachea, preventing complete collapse in certain circumstances.
3. Connective Tissue: The Binding Agent
Surrounding the cartilage rings and trachealis muscle is a network of connective tissues, including elastic fibers and collagen. These tissues:
-
Bind the Cartilage Rings: These tissues act as a "glue", tightly binding the cartilage rings together, maintaining the overall structural integrity of the trachea.
-
Provide Elasticity and Recoil: Elastic fibers confer elasticity to the tracheal wall, allowing it to return to its resting shape after expansion or contraction.
-
Resist Excessive Expansion: Collagen fibers add tensile strength, preventing excessive expansion of the tracheal wall during inspiration.
Biomechanical Principles: Maintaining Tracheal Patency
The trachea's structural components interact in complex ways to maintain patency. Several biomechanical principles are at play:
1. Hoop Stress: The Cartilage Rings' Strength
The hoop stress generated by the C-shaped cartilage rings is the primary mechanism preventing tracheal collapse. Hoop stress refers to the tensile stress within a curved structure, like a ring, that resists radial compression. The rings distribute the pressure exerted on the tracheal walls during respiration, reducing the likelihood of collapse.
2. Negative Intrathoracic Pressure: A Potential Threat, But Also A Factor of Stability
During inspiration, the diaphragm contracts, expanding the thoracic cavity and creating negative intrathoracic pressure. While this pressure is crucial for lung inflation, it also creates an outward force on the chest wall and inward force on the trachea, potentially leading to collapse. However, the rigid cartilage rings effectively resist this inward force.
3. Transmural Pressure: The Balance of Forces
The transmural pressure, the difference between the pressure within the trachea and the pressure outside it, plays a key role in tracheal patency. During normal breathing, the transmural pressure is positive, meaning the internal pressure exceeds the external pressure. This positive pressure helps maintain an open lumen. During forceful exhalation, the transmural pressure can become negative, but the structural support provided by the cartilage rings and trachealis muscle prevents collapse.
Physiological Factors and Potential Risks of Collapse
While the anatomical and biomechanical features generally ensure tracheal patency, several physiological factors and conditions can compromise its integrity, increasing the risk of collapse:
1. Age-Related Changes: Weakening Tissues
With age, the cartilage rings can lose their rigidity and the connective tissues weaken, reducing the trachea's structural support. This age-related degeneration increases the susceptibility to tracheal collapse, particularly during forceful exhalations.
2. Respiratory Diseases: Compromised Function
Chronic obstructive pulmonary disease (COPD), including emphysema and chronic bronchitis, can significantly weaken the tracheal support structures. The increased airway pressures and chronic inflammation associated with COPD can lead to tracheal collapse or stenosis (narrowing).
3. Tracheomalacia: Developmental Abnormality
Tracheomalacia is a condition characterized by excessive flexibility or weakness in the tracheal walls. In this condition, the cartilaginous rings are incompletely formed or abnormally soft, making the trachea prone to collapse, especially during exhalation.
4. External Compression: Pressure from Surrounding Structures
Tumors, enlarged lymph nodes, or other masses pressing on the trachea from the outside can compress the airway, potentially causing stenosis or collapse.
Conclusion: A Complex Interplay for Respiratory Health
The prevention of tracheal collapse is a testament to the intricate interplay of structural design, biomechanical principles, and physiological mechanisms. The C-shaped cartilage rings, trachealis muscle, and connective tissues work together, leveraging hoop stress and resisting transmural pressure fluctuations to maintain an open airway. However, age-related changes and various respiratory diseases can compromise this finely tuned system, emphasizing the importance of understanding the factors that contribute to tracheal patency. Continued research into the biomechanics of the trachea and the development of effective treatments for conditions that compromise its structural integrity remains crucial for ensuring optimal respiratory health.
Latest Posts
Latest Posts
-
How Are Photosynthesis And Cellular Respiration Connected
Mar 05, 2025
-
How To Spell The Number 12
Mar 05, 2025
-
What Are All Of The Factors Of 50
Mar 05, 2025
-
What Is 4 7 As A Percentage
Mar 05, 2025
-
Lowest Common Multiple Of 12 And 7
Mar 05, 2025
Related Post
Thank you for visiting our website which covers about What Prevents The Trachea From Collapsing . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
