Atrioventricular Valves Prevent Backflow Into The
Juapaving
Mar 18, 2025 · 7 min read
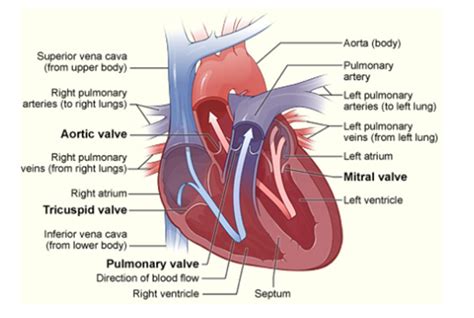
Table of Contents
Atrioventricular Valves: Preventing Backflow and Ensuring Efficient Cardiac Function
The human heart, a tireless powerhouse, pumps blood continuously throughout the body. This intricate process relies on a series of precisely coordinated contractions and relaxations, facilitated by a network of specialized tissues and structures. Central to this system are the atrioventricular (AV) valves, crucial components that ensure unidirectional blood flow and prevent potentially fatal backflow. Understanding their structure, function, and the consequences of their malfunction is essential to appreciating the complexity and delicate balance of the cardiovascular system.
The Role of Atrioventricular Valves in the Cardiac Cycle
The heart's four chambers – two atria and two ventricles – work in a synchronized rhythm. The AV valves act as one-way gates, controlling the flow of blood between the atria and the ventricles. There are two AV valves:
- The tricuspid valve: Located between the right atrium and the right ventricle. As its name suggests, it possesses three cusps (leaflets) of connective tissue.
- The mitral valve (bicuspid valve): Situated between the left atrium and the left ventricle. This valve has two cusps.
These valves open and close passively, responding to pressure changes within the heart chambers during the cardiac cycle. The coordinated actions of these valves are crucial for maintaining the proper sequence of blood flow.
Diastole: Filling the Ventricles
During diastole, the relaxation phase of the cardiac cycle, the atria contract, increasing pressure within the atria. This higher atrial pressure forces the AV valves open, allowing blood to flow passively from the atria into the ventricles. The ventricles fill, preparing for the upcoming contraction. The tricuspid valve allows oxygen-poor blood from the right atrium to fill the right ventricle, while the mitral valve allows oxygen-rich blood from the left atrium to fill the left ventricle. This passive filling is the primary mechanism of ventricular filling.
Systole: Preventing Backflow
When the ventricles contract (systole), the pressure within the ventricles rapidly increases. This increased ventricular pressure forces the AV valves to close. This closure is essential to prevent the backflow of blood from the ventricles into the atria. The forceful closure of the AV valves produces the familiar "lub" sound heard during auscultation (listening to the heart with a stethoscope). The closure of the AV valves is a crucial step to ensuring that blood is effectively propelled forward into the pulmonary artery (from the right ventricle) and the aorta (from the left ventricle).
The Structure of Atrioventricular Valves: A Closer Look
The AV valves are not simply flaps of tissue; they have a sophisticated structure that contributes to their efficient function:
- Cusps (leaflets): Made of strong, fibrous connective tissue covered by a thin layer of endothelium (the inner lining of blood vessels and the heart). The cusps are arranged to ensure a tight seal when closed.
- Chordae tendineae: These are tough, fibrous cords that attach to the free edges of the AV valve cusps. They resemble tiny strings or tendons.
- Papillary muscles: These are cone-shaped muscles located within the ventricular walls. The chordae tendineae are attached to the papillary muscles.
The chordae tendineae and papillary muscles work together to prevent the AV valve cusps from inverting (prolapsing) into the atria during ventricular contraction. When the ventricles contract, the papillary muscles contract simultaneously, tightening the chordae tendineae and preventing the cusps from being pushed back into the atria. This coordinated action ensures a complete seal, preventing regurgitation (backflow) of blood.
Consequences of Atrioventricular Valve Dysfunction
When the AV valves fail to function properly, several serious cardiovascular problems can arise:
Mitral Valve Prolapse (MVP)
MVP is a condition where one or both mitral valve leaflets bulge (prolapse) back into the left atrium during ventricular contraction. This can lead to mitral regurgitation, where blood flows back from the left ventricle into the left atrium. Symptoms can range from none to shortness of breath, fatigue, and palpitations. In severe cases, MVP can cause heart failure.
Mitral Regurgitation
This condition involves the incomplete closure of the mitral valve, allowing blood to leak back into the left atrium during ventricular systole. The severity depends on the extent of the leakage. Symptoms may include shortness of breath, fatigue, and dizziness. Untreated mitral regurgitation can lead to heart failure and other complications.
Tricuspid Regurgitation
Similar to mitral regurgitation, tricuspid regurgitation involves the incomplete closure of the tricuspid valve, allowing blood to flow back into the right atrium during right ventricular contraction. This condition is often associated with other heart conditions. Symptoms can include shortness of breath, edema (swelling), and fatigue.
Atrioventricular Valve Stenosis
Stenosis refers to the narrowing of a valve opening. AV valve stenosis restricts blood flow from the atrium to the ventricle, increasing the workload on the heart. Symptoms can include shortness of breath, chest pain, and dizziness. Severe stenosis can lead to heart failure.
Causes of Atrioventricular Valve Disease
Several factors can contribute to AV valve dysfunction:
- Congenital heart defects: Some individuals are born with malformed or abnormal AV valves.
- Infective endocarditis: Infection of the heart valves can damage the valve leaflets, leading to regurgitation or stenosis.
- Rheumatic fever: A complication of strep throat, rheumatic fever can cause inflammation and scarring of the heart valves.
- Degeneration: AV valves can degenerate over time, becoming stiffer and less flexible. This is more common in older adults.
- Myocardial infarction (heart attack): Damage to the heart muscle can affect the function of the papillary muscles and chordae tendineae, leading to valve dysfunction.
- Connective tissue disorders: Conditions like Marfan syndrome can weaken the connective tissue of the heart valves, increasing the risk of prolapse or regurgitation.
Diagnosis and Treatment of Atrioventricular Valve Disease
Diagnosis of AV valve disease often involves a combination of:
- Physical examination: Listening to the heart with a stethoscope (auscultation) can reveal murmurs, abnormal heart sounds indicative of valve problems.
- Electrocardiogram (ECG): An ECG measures the heart's electrical activity, providing insights into the heart's rhythm and potential abnormalities.
- Echocardiogram: An echocardiogram uses ultrasound to create images of the heart and its valves, allowing for detailed assessment of valve structure and function. This is the gold standard for diagnosing AV valve diseases.
- Cardiac catheterization: In some cases, cardiac catheterization, a more invasive procedure, may be necessary to obtain more detailed information about the severity of the valve problem.
Treatment options for AV valve disease depend on the severity of the condition and the specific valve involved. Options may include:
- Medications: Medications may be used to manage symptoms such as heart failure or high blood pressure.
- Valve repair: In some cases, the damaged valve can be repaired surgically, restoring its function. This is often the preferred option when possible, as it preserves the patient's own valve.
- Valve replacement: If the valve is severely damaged or cannot be repaired, it may need to be replaced with a prosthetic valve. Prosthetic valves can be either mechanical or biological. Mechanical valves are durable but require lifelong anticoagulation therapy (blood thinners) to prevent blood clots. Biological valves are less durable but do not require anticoagulation.
The choice between valve repair and replacement is a complex decision that depends on various factors, including the patient's age, overall health, and the severity of the valve disease. The decision is typically made collaboratively between the patient and their cardiologist.
Conclusion: The Vital Role of Atrioventricular Valves
The atrioventricular valves, despite their seemingly simple structure, play a pivotal role in maintaining the unidirectional flow of blood through the heart. Their precise function is crucial for efficient cardiac output and overall cardiovascular health. Understanding the structure, function, and potential malfunctions of these valves is paramount in appreciating the intricate mechanisms that govern the human circulatory system. Early diagnosis and appropriate treatment of AV valve disease are vital to prevent life-threatening complications and improve the quality of life for affected individuals. The prevention of cardiac disease through lifestyle choices such as regular exercise, a balanced diet, and avoiding smoking, along with prompt medical attention for any cardiac symptoms, are crucial steps in preserving cardiovascular health.
Latest Posts
Latest Posts
-
In What Direction Does A Liquid Exert Force
Mar 18, 2025
-
Non Metal Liquid At Room Temperature
Mar 18, 2025
-
Common Factors Of 20 And 35
Mar 18, 2025
-
How Do You Turn A Gas Into A Liquid
Mar 18, 2025
-
The Purpose Of Residual Air In The Lungs Is To
Mar 18, 2025
Related Post
Thank you for visiting our website which covers about Atrioventricular Valves Prevent Backflow Into The . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
