A Plasma Protein Essential For Blood Clotting Is
Juapaving
Mar 24, 2025 · 6 min read
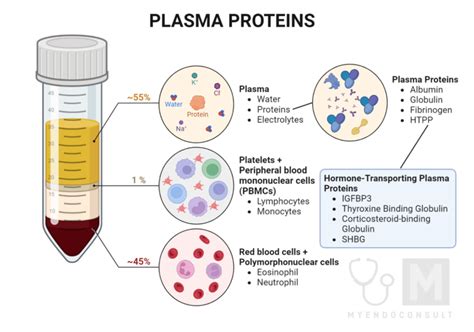
Table of Contents
Fibrinogen: A Plasma Protein Essential for Blood Clotting
Fibrinogen, a crucial plasma protein, plays a pivotal role in the complex process of hemostasis, ultimately leading to blood clot formation. Understanding its structure, function, and regulation is fundamental to comprehending the intricate mechanisms that prevent excessive bleeding and maintain vascular integrity. This comprehensive article delves deep into the world of fibrinogen, exploring its multifaceted nature and clinical significance.
Understanding the Structure of Fibrinogen
Fibrinogen, a glycoprotein, boasts a unique and intricate structure. Its molecular weight is approximately 340 kDa, and it exists as a dimer composed of two sets of three polypeptide chains: Aα, Bβ, and γ. These chains are linked by disulfide bonds, creating a symmetrical, elongated structure often described as resembling a "dimer of trimers." Each half of the fibrinogen molecule comprises three coiled domains, held together by non-covalent interactions.
The Three Domains: A Closer Look
Each half of the fibrinogen molecule features three distinct domains:
-
D-domains (Distal domains): These domains are located at the ends of the molecule and are responsible for the initial polymerization process during clot formation. They contain specific binding sites that facilitate the interaction with other fibrinogen molecules and with the fibrinolytic system components.
-
E-domain (Central domain): Situated in the central region of the molecule, the E-domain is crucial for connecting the two D-domains and plays a vital role in maintaining the overall structure of the fibrinogen molecule. It also contains binding sites for various other proteins involved in coagulation.
-
Connecting domains: The connecting domains serve as the linkage between the D-domains and the E-domain. These domains are essential for maintaining the overall molecular shape and stability of fibrinogen.
Fibrinogen's Role in Blood Clotting: The Cascade of Events
Fibrinogen's primary function is to convert into fibrin, the insoluble protein that forms the meshwork of a blood clot. This conversion is triggered by a series of enzymatic reactions, collectively known as the coagulation cascade. The process can be broadly summarized as follows:
-
Injury to a blood vessel: When a blood vessel is injured, the underlying collagen is exposed, triggering a cascade of events.
-
Activation of coagulation factors: This exposure activates various coagulation factors, leading to the formation of thrombin, a serine protease.
-
Thrombin's action on fibrinogen: Thrombin acts as a specific enzyme, cleaving off small fibrinopeptides A and B from the fibrinogen molecule. This cleavage exposes polymerization sites, leading to the formation of fibrin monomers.
-
Fibrin monomer polymerization: The fibrin monomers spontaneously assemble into long, insoluble fibrin polymers, forming a mesh-like structure.
-
Crosslinking and stabilization: Factor XIIIa, a transglutaminase enzyme activated during the coagulation cascade, crosslinks the fibrin polymers, solidifying and stabilizing the clot structure, enhancing its strength and durability. This forms a stable, insoluble fibrin clot, effectively stemming the bleeding.
Regulation of Fibrinogen Production and Levels
The liver is the primary site of fibrinogen synthesis. Its production is tightly regulated by a variety of factors, including:
-
Inflammation: During inflammatory processes, the production of fibrinogen significantly increases, contributing to the acute-phase response. This increased production helps in the formation of clots at the site of inflammation or injury. This is a crucial aspect of the body's defense mechanism against infection and injury.
-
Hormonal influences: Hormones such as estrogen and thyroid hormones have been shown to influence fibrinogen levels.
-
Nutritional status: Adequate dietary intake of essential amino acids, vitamins, and minerals is necessary for optimal fibrinogen synthesis.
-
Genetic factors: Genetic variations can influence fibrinogen production and levels, increasing or decreasing susceptibility to thrombotic or bleeding disorders.
Clinical Significance of Fibrinogen: Conditions and Implications
Fibrinogen levels are clinically relevant indicators of health and disease. Both abnormally high and low levels can signal underlying medical conditions:
Hyperfibrinogenemia: Elevated Fibrinogen Levels
Elevated fibrinogen levels, known as hyperfibrinogenemia, are often associated with:
-
Inflammation: Chronic inflammatory conditions like rheumatoid arthritis, Crohn's disease, and systemic lupus erythematosus commonly present with increased fibrinogen levels.
-
Pregnancy: Fibrinogen levels naturally rise during pregnancy, as part of the physiological response to maintain hemostasis.
-
Cardiovascular disease: Hyperfibrinogenemia is a well-established risk factor for cardiovascular disease, including stroke, myocardial infarction, and deep vein thrombosis (DVT). The increased propensity for clot formation elevates the risk of these conditions.
-
Cancer: Several types of cancer can cause increased fibrinogen production as part of the body's general inflammatory response.
-
Obesity: Elevated fibrinogen levels are frequently observed in individuals with obesity, partially attributed to the underlying inflammation and metabolic disturbances.
Hypofibrinogenemia: Low Fibrinogen Levels
Low fibrinogen levels, called hypofibrinogenemia, represent a significant risk of uncontrolled bleeding, and can result from:
-
Liver disease: Since the liver synthesizes fibrinogen, liver dysfunction severely impacts fibrinogen production. Conditions like cirrhosis and hepatitis can lead to decreased fibrinogen levels.
-
Disseminated intravascular coagulation (DIC): DIC is a pathological condition characterized by widespread clotting and activation of the coagulation system, eventually leading to consumption of clotting factors, including fibrinogen.
-
Congenital fibrinogen disorders: Rare genetic defects can cause deficiencies in fibrinogen production or abnormal fibrinogen function.
-
Severe infections: Overwhelming infections can exhaust the body's ability to produce fibrinogen.
-
Certain medications: Some medications can interfere with fibrinogen production or function.
Diagnostic Testing for Fibrinogen
Measuring fibrinogen levels is a routine part of blood tests. Common methods include:
-
Clauss method: A widely used method that measures the clotting time of plasma following the addition of thrombin. It provides a quantitative assessment of fibrinogen levels.
-
Immunoturbidimetric assay: This method measures fibrinogen antigen levels using antibodies specific to fibrinogen. It offers a rapid and accurate means of measuring fibrinogen.
Therapeutic Implications: Treatments and Management
Treatment strategies for abnormal fibrinogen levels depend largely on the underlying cause and the severity of the symptoms. For instance:
-
Treating the underlying condition: Addressing the underlying cause of hyperfibrinogenemia or hypofibrinogenemia often helps normalize fibrinogen levels.
-
Anticoagulation therapy: Individuals with hyperfibrinogenemia and a high risk of thrombotic events may benefit from anticoagulant therapy to prevent clot formation.
-
Fibrinogen replacement therapy: Hypofibrinogenemia may require fibrinogen replacement therapy, which involves intravenous administration of fibrinogen concentrates to restore normal levels.
-
Lifestyle modifications: Lifestyle modifications, such as diet and exercise, play a supportive role in managing hyperfibrinogenemia and other associated risk factors.
Future Directions in Fibrinogen Research
Ongoing research continues to unravel the complexities of fibrinogen, its regulation, and its involvement in various pathological conditions. Future research focuses on:
-
Developing more targeted therapies: Researchers are actively pursuing novel therapies that specifically target fibrinogen pathways, enabling more precise and effective treatment of thrombotic and bleeding disorders.
-
Improved diagnostic tools: Efforts are underway to develop more sensitive and specific assays to measure fibrinogen levels and to identify variations in fibrinogen structure and function.
-
Personalized medicine approaches: Tailoring treatment strategies based on individual characteristics, including genetic predisposition and disease severity, holds great promise for improving outcomes in patients with fibrinogen-related disorders.
Conclusion
Fibrinogen stands as a pivotal protein in maintaining hemostasis and preventing excessive bleeding. Its intricate structure, complex interactions within the coagulation cascade, and its profound impact on health and disease make it a central focus of ongoing research. A deep understanding of fibrinogen's role is crucial for effective diagnosis, treatment, and management of various clinical conditions. This detailed exploration has provided a robust understanding of fibrinogen, its function, associated conditions, and implications for human health. Further research will undoubtedly unveil additional insights into this vital protein and its role in maintaining overall health.
Latest Posts
Latest Posts
-
One Cubic Foot Is How Many Gallons
Mar 28, 2025
-
How Many Centimeters Is 5 Foot
Mar 28, 2025
-
Five Letter Words Starting With Hea
Mar 28, 2025
-
Difference Between Bony Fish And Cartilaginous Fish
Mar 28, 2025
-
The Scattering Of Light By Colloidal Particles
Mar 28, 2025
Related Post
Thank you for visiting our website which covers about A Plasma Protein Essential For Blood Clotting Is . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
